ASCO: Ibrutinib Shows Promise as First-Line Treatment in Elderly CLL Patients
Impressive interim results from a phase Ib/II trial of ibrutinib, a selective Bruton tyrosine kinase inhibitor, in patients with chronic lymphocytic leukemia (CLL) were reported at ASCO.
CHICAGO-Impressive interim results from a phase Ib/II trial of ibrutinib (formerly PCI-32765), a selective Bruton tyrosine kinase inhibitor (TKI), in patients with chronic lymphocytic leukemia (CLL) were reported by John C. Byrd, MD, of the division of hematology, Ohio State University Comprehensive Cancer Center, Columbus.[1] Dr. Byrd presented findings derived from a subset of elderly treatment-naive patients. Results in patients with relapsed or refractory disease were reported at the 2011 annual meeting of the American Society of Hematology by Susan M. O'Brien, MD, of the M.D. Anderson Cancer Center in Houston. Byrd and O’Brien are lead investigators of the multicenter trial, composed of a variety of 117 patients with CLL, treated at different dose levels of ibrutinib.
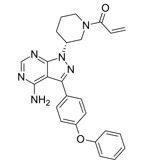
Chemical structure of ibrutinib
The treatment-naive subset included a total of 31 patients aged 65 to 84 years (the median age was 71 years) with CLL/small lymphocytic leukemia (SLL). Patients were treated at two fixed continuous dose levels of ibrutinib, 420 mg (26 patients) and 840 mg (5 patients), respectively. Primary objectives were safety, response rate, and progression-free survival.
Treatment at the higher dose was discontinued after 7.4 months “because when we looked back at the patients who had prior therapy there was one hundred percent Bruton TK occupancy at the lower dose, and the responses and toxicity appeared to be the same, so it didn’t make sense to continue using the higher dose,” explained Dr. Byrd.
With a median follow-up of 14.4 months in the 420 mg cohort, the overall response rate, including complete and partial responses, was 81% as measured by the 2008 International Workshop on Chronic Lymphocytic Leukemia (IWCLL) criteria. Another 12% (3 of the 26 patients) achieved “nodal responses” with lymphocytosis, which cannot be classified as partial responses under existing IWCLL criteria. Nodal response describes patients who achieved a partial response by other parameters until a 50% reduction in absolute lymphocyte count or an absolute lymphocyte count less than 5K was attained. Progression-free survival in the 420-mg cohort was 96%. Clinical responses have been independent of high-risk clinical or genetic features, said Dr. Byrd. Twelve percent of patients achieved a complete response with no morphologic evidence of CLL.
As in earlier trials, the safety profile of ibrutinib was notable for minimal off-target toxicities, Dr. Byrd observed. A majority of adverse events were grade 2 or lower, including diarrhea, nausea, and fatigue. Of the 31 patients on the trial, only one has discontinued due to disease progression.
Combination Trials
Interim data from two trials investigating ibrutinib in combination with other agents were also presented at ASCO. Initial safety and efficacy data from a phase Ib/II trial of ibrutinib in combination with ofatumumab (Arzerra), an anti-CD20 monoclonal antibody, for treatment of CLL/SLL and related disease were reported by Samantha Mary Jaglowski, MD, also from the division of hematology, Ohio State University Comprehensive Cancer Center, Columbus.[2] The trial included a total of 27 patients with CLL/SLL and prolymphocytic leukemia (PLL) (24 patients), and Richter transformation (3 patients). In this ongoing trial patients with relapsed/refractory CLL/SLL who have received two or more prior therapies are treated with ibrutinib (420 mg) daily until disease progression, followed by concomitant ofatumumab with continued ibrutinib until progression.
For the CLL/SLL/PLL patients the overall response rate, as measured by IWCLL criteria and progression-free survival is 100%, with a median follow-up of 9.8 months; 89% of CLL/SLL/PLL patients remain on study and only one patient has discontinued treatment by proceeding to stem cell transplant. The majority of adverse events were grades 1 or 2, and no grade 3 or 4 infusion reactions, neutropenia, or thrombocytopenia have been observed. “The combination was well tolerated and highly active in patients with heavily pretreated relapsed/refractory CLL/SLL,” said Dr. Jaglowski. “Rapid onset of response, low relapse rate, and favorable safety profile make this combination worthy of further study.”
Similar results have been achieved thus far in a phase Ib/II trial of ibrutinib in combination with bendamustine (Treanda) and rituximab (Rituxan) in patients with relapsed and refractory CLL, findings of which were reported by Dr. O’Brien. The trial enrolled a total of 30 patients; 37% were considered refractory to a purine analog-containing regimen and 13% refractory to bendamustine. With a median follow up of 8.1 months only two patients have reported progressive disease and an additional five patients have proceeded to stem cell transplant; 23 patients (77%) remain on study, said Dr. O’Brien. Overall response rate is 93%, with 13% of patients achieving a complete response with no morphologic evidence of CLL.
“Ibrutinib in combination with bendamustine and rituximab, is highly active,” Dr. O’Brien concluded. “The high overall response rate, low rate of progressive disease, and good tolerability compares very favorably with historical controls, warranting additional investigation of this combination."
“We now have a drug that is easy to take, that you can take long term, appears to suppress the disease long term, and appears not to be associated with resistance,” said Constantine Tam, MD, of St. Vincent’s Hospital, Melbourne, commenting on the findings of the ibrutinib trials. “For older patients we now have a chance for nonchemotherapy treatment, with indefinite suppression of this disease. The caveat is that the data are still early.”
"This meeting at ASCO has been a continued affirmation of the promising activity and clinical benefit of ibrutinib in CLL,” said Dr. Byrd. “It will be exciting to move this toward definitive phase III study to get this drug approved for CLL patients.”
References
1. O'Brien SM, Barrientos JC, Flinn IW, et al. Combination of the Bruton's tyrosine kinase (BTK) inhibitor PCI-32765 with bendamustine (B)/rituximab (R) (BR) in patients (pts) with relapsed/refractory (R/R) chronic lymphocytic leukemia (CLL): Interim results of a phase Ib/II study. J Clin Oncol. 2012;30:(suppl; abstr 6515).
2. Jaglowski SM, Jones JA, Flynn JM, et al. A phase Ib/II study evaluating activity and tolerability of BTK inhibitor PCI-32765 and ofatumumab in patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and related diseases. J Clin Oncol. 2012;30:(suppl; abstr 6508).