Bacterial Infections in Patients With Solid Tumors
Early and appropriate management of infection in the patient with cancer is critical to optimizing patient outcomes.
ABSTRACT: The employment of best practices is essential for minimizing the disease burden of cancer and optimizing patient outcomes. However, areas of clinical confusion remain and patients continue to receive inappropriate therapies. The aim of this article is to present key evidence-based strategies for initial assessment, early management, and prevention of bacterial infection in patients with common solid tumors. First, the need for astute clinical assessment, including risk assessment and symptom-based diagnostic testing, will be discussed. Then, the selection of therapeutics for early intervention will be outlined, along with key nursing considerations regarding monitoring for toxicities. The efficacy of innovations, such as antimicrobial central venous catheters, will also be reviewed. Recommendations are based on practice guidelines from the National Comprehensive Cancer Network, Infectious Diseases Society of America, Healthcare Infection Control Practices Advisory Committee, Centers for Disease Control and Prevention, Surviving Sepsis Campaign, and Oncology Nursing Society.

Early and appropriate management of infection in the patient with cancer is critical to optimizing patient outcomes. Practices that are not recommended by current guidelines continue to be used frequently, however.[1] Examples include routine fluoroquinolone prophylaxis, reactive use of colony-stimulating factors, and inappropriate selection of anti-infectives for empiric therapy in low-risk patients. The purpose of this article is to summarize pharmacologic and nonpharmacologic management and prevention strategies for bacterial infection in adult patients with solid tumors. For prevention and management strategies for fungal and viral processes in both solid tumors and hematologic malignancies, readers are referred to guidelines from the National Comprehensive Cancer Network (NCCN), Infectious Diseases Society of America (IDSA), and Centers for Disease Control and Prevention (CDC).
Patients with cancer are at increased risk of infection and at greater risk of complications from infectious processes. Multiple factors escalate their susceptibility: the absence of granulocytes; disruption of integumentary, mucosal, and mucociliary barriers; foreign devices such as vascular catheters; nutritional deficiencies; and pre-existing or newly acquired comorbidities.[2,3] Timely and effective management of infection increases the likelihood of timely receipt of anticancer therapies, decreased disease burden and symptom distress, and enhanced quality of life. In this article, we will focus first on initial assessment and interventions, and will conclude with a summary of strategies for prevention of infection.
Initial Assessment
Early management of an infectious process is of utmost importance in the patient with cancer, to decrease the risk of sepsis and related complications. The NCCN defines neutropenia as either (1) an absolute neutrophil count (ANC) < 500/ L, or (2) an ANC < 1,000/ L and a predicted decline to 500/ L over the next 48 hours. Fever is defined as a single temperature of 38.3°C (about 101°F) or higher orally or of 38.0°C (100.4°F) or higher lasting longer than 1 hour in the absence of an obvious cause.[3]
FIGURE 1

Fever and Infection-Initial Assessment, Intervention, and Evaluation. Information adapted from Reference 3.
Signs and symptoms of an infection may be muted or absent when neutropenia is present. Fever remains an early sign, however.[4] Approximately 40% of patients who become febrile have an established or occult infection,[5] whereas 57% of patients with cancer in a large national observational study did not have a documented source of infection.[6] Initial evaluation of a patient with fever should begin with a site-specific history and complete physical examination, with a focus on determining the potential site and causative organisms of infection, plus the patient's risk of developing a related complication (Figure 1). High-risk patients include those with the following conditions:
• Clinically unstable at presentation;
• Significant medical comorbidity;
• Anticipated prolonged severe neutropenia (100 cells/ L for 7 days);
• Hepatic insufficiency (aminotransferase levels five times ULN [upper limit of normal]);
• Renal insufficiency (creatinine clearance < 30 mL/min);
• Uncontrolled or progressive cancer;
• Pneumonia or other complex infection on presentation;
• Oral mucositis grade 3–4; and/or
• Multinational Association for Supportive Care in Cancer (MASCC) Risk Index score < 21.
These high-risk patients should be referred to a hospital for intravenous anti-infective therapy and close monitoring for response. Low-risk patients, for whom treatment at an ambulatory clinic may be appropriate, include those with:
• No associated acute comorbid illness that requires inpatient treatment or close observation;
• Anticipated short duration of severe neutropenia (100 cells/ L for < 7 days);
• Good performance status (ECOG [Eastern Cooperative Oncology Group] score of 0–1);
• No hepatic insufficiency;
• No renal insufficiency; and/or
• MASCC Risk Index score 21.[3]
In predicting risk in febrile neutropenic cancer patients, the MASCC Risk Index[7] assigns weighted numerical values to variables such as burden of illness (signs or symptoms at presentation), hypotension, chronic obstructive pulmonary disease (COPD), solid tumor or hematologic malignancy, history of previous fungal infection, dehydration, outpatient status, and age. The score predicts the probability that a patient will experience serious complications. It may also be used as a guide to determine whether the patient is a candidate for outpatient management with oral antibiotics.
Laboratory Data
Initial laboratory tests should include a complete blood count with differential analysis, platelets, blood urea nitrogen, creatinine, electrolytes, total serum bilirubin, and liver-associated enzymes. Chest radiographs should be taken for all patients with respiratory signs or symptoms. A source of infection may not be evident in neutropenic patients with pulmonary infection, however. A computerized tomography (CT) scan of the chest may be more effective in detecting a source of infection.
Culture specimens should be collected during or immediately after completing the history and physical examination. It is essential that the samples be collected prior to the initiation of antibiotic therapy; there is concern regarding the potential for lower yields from cultures if antibiotics are provided prior to culture collection. Two sets of blood cultures should be obtained. (Each set consists of two bottles: one aerobic sample and one anaerobic sample.) If the patient has a vascular access device (VAD), the NCCN panel recommends obtaining one sample from the catheter and one sample peripherally. This may be helpful in determining whether the VAD is the source of infection based on the differential time to positivity.[8] Alternatively, both sets can be obtained peripherally or through the catheter. The positive predictive value of catheter cultures is lower than that of peripheral cultures. If a patient is suspected to have a catheter-related bloodstream infection (CRBSI) and a blood sample cannot be drawn from a peripheral vein, the IDSA recommends that two or more blood samples be drawn from different catheter lumens. It is unclear whether blood samples should be drawn from all catheter lumens in such cases. The need for samples from both peripheral and central sites also remains unclear at this time. The NCCN panel consensus is that the volume of blood for culture is the most important aspect of blood culturing. The recommended volume is 20–30 mL.[9]
The NCCN panel states that routine cultures of the urine, stool, rectum, anterior nares, and oropharynx are rarely helpful in the absence of lesions or clinical signs and symptoms. In the presence of diarrhea, however, stools should be tested for the presence of Clostridium difficile.[10] Especially in the winter months and during outbreaks, diarrheal stools should be tested for rotavirus and norovirus, as part of the differential diagnosis. A urinalysis and urine culture should be done in the presence of symptoms of urinary tract infection; microbiologic and pathologic evaluations should be performed for new and undiagnosed skin lesions; and viral cultures and rapid viral antigen testing of nasopharyngeal secretions can be useful in evaluating respiratory viral symptoms. It must be noted, however, that inability to mount an effective inflammatory response may decrease the reliability of some laboratory tests.[2] One study from the 1970s found that 40% of neutropenic patients with pneumonia had a normal chest radiograph and only 8% of patients had sputum Gram stains revealing polymorphonuclear cells.[11] In more recent research investigators have emphasized that while pneumonia in febrile neutropenic patients needs to be diagnosed as early as possible, conventional chest radiographs often fail to detect lung infiltrates at an early stage in these patients, “meaning that a normal chest radiograph must be interpreted with caution,” and recommending thoracic computed tomography (CT) scans in this setting.[12]
Pharmacological Interventions
Because currently available diagnostic tests are not rapid, sensitive, or specific enough to enable tailored treatment, all neutropenic patients who demonstrate signs of infection (ie, fever) should receive prompt empiric therapy-the early provision of treatment for a presumed infection-with broad-spectrum antibiotics. Mortality risks are lower when patients receive early empiric therapy.[13] In selecting initial therapy, the most common pathogens should be considered. Initial infections early in the course of fever and neutropenia are caused largely by bacteria. Antibiotic-resistant bacteria, yeast, other fungi, and viruses are often causes of infections that occur later in the clinical course. If a patient has been hospitalized recently, antimicrobial susceptibilities of pathogens causing infection in the facility should also be considered.[3]
For antimicrobial treatment of a low-risk patient in the outpatient setting, ciprofloxacin with amoxicillin/clavulanate (500 mg each every 8 hours) is considered the current oral regimen of choice.[3] Anti-infective choice in these patients should have strong coverage for gram-negative bacilli, specifically Pseudomonas aeruginosa, and other gram-negative infections prevalent in the local community. For patients who are allergic to penicillin, ciprofloxacin plus clindamycin is an acceptable alternative. Ciprofloxacin monotherapy is not recommended by the NCCN panel, owing to the potential for serious breakthrough Streptococcus viridans infections.
TABLE 1
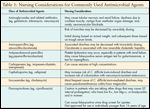
Nursing Considerations for Commonly Used Antimicrobial Agents
Daily follow-up of a patient treated in the outpatient setting is recommended while the patient is febrile. Return to clinic is recommended for any positive culture, persistent or recurrent fever at 3–5 days, development of serious subsequent infection or an adverse event, or if the patient is unable to continue to receive or tolerate the prescribed antibiotic regimen. Some antimicrobial agents require closer monitoring for toxicities. Table 1 highlights these considerations.
For hospitalized patients with high-risk features, the NCCN panel has endorsed multiple agents for consideration based on large, randomized controlled clinical trials.[4,13,14] The first approach is intravenous (IV) antibiotic monotherapy with either imipenem/cilastatin (Primaxin), meropenem (Merrem), or piperacillin/tazobactam (Zosyn). Although cefepime was reported in a meta-analysis of randomized trials to increase all-cause mortality when used as empiric therapy for neutropenic fever,[15,16] a recent meta-analysis by the US Food and Drug Administration (FDA) did not find a statistically significant increase in mortality for cefepime-treated patients, compared with controls. The FDA has concluded, therefore, that cefepime remains appropriate therapy for its approved indications, and it continues to monitor the safety of this agent.
Another approach recommended by NCCN is IV antibiotic combination therapy using three options: (1) an aminoglycoside plus an antipseudomonal penicillin (with or without a beta-lactamase inhibitor); (2) ciprofloxacin plus an antipseudomonal penicillin[17]; or (3) an aminoglycoside plus an extended-spectrum antipseudomonal cephalosporin (ceftazidime or cefepime).[17–19]
Routine use of vancomycin is strongly discouraged because of the increased frequency of beta-lactam–resistant gram-positive infections. Considerations for vancomycin use include clinical instability, apparent CRBSI, documented gram-positive pathogens, history of resistant pneumococci or methicillin-resistant Staphylococcus aureus (MRSA), soft tissue infection, and severe mucositis. If empiric vancomycin is initiated, use should be re-evaluated in 2 to 3 days. Discontinuation should be considered if no resistant gram-positive pathogen is identified. The NCCN panel advises practitioners to follow the recommendation of the Hospital Infection Control Practices Advisory Committee (HICPAC) of the CDC for preventing the spread of vancomycin resistance.[20,21]
Neutropenic patients who are clinically unstable (those with hypotension, tachypnea, new or worsening tachycardia, mental status changes, decreased urine output, and organ dysfunction) may benefit from initial empiric therapy that includes an aminoglycoside and vancomycin in addition to a broad-spectrum beta-lactam. The NCCN panel recommends giving strong consideration to the addition of fluconazole or an echinocandin in patients not receiving antifungal prophylaxis. The regimen should be modified based on the patient's culture results and susceptibilities. For patients in septic shock requiring vasopressor support, intravenous steroids should be given only to adults whose blood pressure demonstrates poor response to fluid resuscitation and vasopressor therapy.[22] In cases of severe sepsis or septic shock, use of high-dose steroids (comparable to > 300 mg hydrocortisone daily) with intent to treat the septic shock may be detrimental and should be avoided.[22,23]
Response to empiric therapy should be evaluated in 3 to 5 days. Response to treatment may be assessed through repeat blood cultures, monitoring of fever trends, assessment of signs and symptoms of infection, and evaluation of drug-specific toxicities. For patients on prolonged treatment with anti-infectives, renal and hepatic function should be assessed at least twice weekly.
Catheter-Related Bloodstream Infections
CRBSIs are heterogeneous in nature. Common classifications of these infections include geography (entry or exit site, tunnel or port pocket); septic phlebitis, defined as inflammation of a vein as a result of bacterial infection; and catheter-associated. For a clinically apparent tunnel or port pocket infection, or septic phlebitis, blood cultures should be obtained from each port of the VAD, the surgical wound should be cultured, and the catheter removed immediately.[3] Most VAD exit-site infections respond to antimicrobial therapy without the need for catheter removal, but immediate catheter removal is also recommended for patients with bloodstream infections caused by fungi or nontuberculosis mycobacteria.[3] When a VAD is a possible infection source and there is no visibly apparent inflammation at the site, the differential time to positivity (DTP) method may be a useful diagnostic tool and can help the clinician to avoid unnecessary catheter removal.[24] For clinically apparent catheter-related inflammation, tunnel or pocket infection, or septic phlebitis, vancomycin should be added to initial empiric therapy.[3] Additional details about CRBSI prevention and management can be found in the 2009 IDSA guidelines.[24]
Increased focus on the reduction of CRBSIs has led to the use of antibiotic-impregnated catheters, antibiotic flushing techniques, and antibiotic locks in long-term catheters. Antimicrobial central venous catheters (CVCs) have been found to be effective in reducing CRBSIs, although efficacy varies with type of antimicrobial agent.[25,26] Also, variations in the definition and diagnosis of CRBSI, methodology, and quality of studies necessitate further research in this area. Catheters coated with a combination of minocycline and rifampicin have been found to be superior to the majority of catheters coated with other anti-infectives, showing activity against many gram-positive and gram-negative bacteria. At this time, the HICPAC of the CDC recommends use of antimicrobial CVCs in adults who are expected to have the catheter in place longer than 5 days and are receiving care at a hospital that has high CRBSI rates despite having comprehensive preventive strategies in place. Patients receiving antimicrobial catheters should be monitored closely for development of drug resistance.[26] It should be noted that catheters coated with a combination of chlorhexidine and silver sulfadiazine have been found to cause anaphylactic reaction on rare occasions.[27]
Prevention of Infection
TABLE 2

Summary of Preventive Interventions for Bacterial Infection
An ongoing project of the Oncology Nursing Society (ONS), called Putting Evidence into Practice, or ONS-PEP, provides clinical resources with evidence-based recommendations for practice on a variety of topics, based on current research.[28] These are available in multiple formats, including as a quick and easy-to-use one-page summary of interventions, and nurses and patients often can obtain them free of charge. Interventions are classified as recommended for practice, likely to be effective, benefits balanced with harms, effectiveness not established, effectiveness unlikely, and not recommended for practice. PEP strategies related to the prevention of bacterial infection, classified into these categories, can be found in Table 2.
When cleaning equipment and other surfaces that may have been contaminated with C. difficile, dilute solutions of 5.25%–6.15% sodium hypochlorite (eg, a 1:10 dilution of household bleach) are recommended for disinfection.[29] There is concern about proliferation of C. difficile spores with exposure to nonchlorine-based cleaning agents, and commonly used surface disinfectants may not be sufficient to kill resistant spores.[30] Further studies are warranted with regard to the effectiveness of routine surveillance cultures. Many studies are methodologically flawed, which threatens the validity of reported outcomes.[31]
Handwashing
It is clear that proper hand hygiene is the most effective way to prevent infections.[32] As a result of increased vigilance to reduce healthcare-associated infections (HAIs), it is assumed that readers are very familiar with strategies for effective hand hygiene. Details of hand hygiene guidelines are available from the CDC based on the recommendations from task forces of major infection-control agencies. Key points from the guidelines are as follows[33]:
• Use soap (either antimicrobial or not antimicrobial) and water for visibly soiled hands; use either soap and water or alcohol-based handrub if hands are not visibly soiled.
• When caring for patients with C. difficile infection, gloves should be worn and soap and water must be used to physically remove spores. (Alcohol-based handrubs are not adequate.)
• Decontaminate hands before and after direct patient contact, donning gloves, and contact with inanimate objects in the immediate vicinity of the patient.
• Allow hands to dry completely after using either soap and water or an alcohol-based handrub.
In trials, alcohol-based handrub appears to reduce microbe counts more dramatically than soap or other gel-based solutions,[34,35] with the exception of hand contamination with C. difficile, for which recent studies have confirmed soap and water to be more effective than alcohol-based handrubs.[36,37] Strategies to increase hand-hygiene effectiveness have been studied extensively. Helpful strategies include: system-level changes to make hand hygiene easy and convenient (eg, ensuring soap availability in dispensers, providing fast access to sinks and alcohol-based handrubs, and choosing cleansers that are least damaging or drying to skin); audit and feedback; patient education and empowerment regarding infection prevention; linking hand hygiene to patient safety; providing rewards; and use of a multimodal approach.[38]
Conclusion
Bacterial infections in patients with cancer remain a significant problem, one which may impede delivery of chemotherapy, hinder quality of life, and increase the risk of morbidity and mortality. We have summarized pivotal studies and recommendations for the management and prevention of infections in these patients. A combination of astute clinical assessment, rapid intervention with appropriate therapies, and monitoring for toxicities, coupled with nonpharmacological strategies, increase the likelihood of optimal patient outcomes.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
Acknowledgement:Dr. Friese is supported by a Pathway to Independence Award (K99 NR010750) from the National Institute of Nursing Research, National Institutes of Health.
References:
References
1. Freifeld A, Sankaranarayanan J, Ullrich F, et al: Clinical practice patterns of managing low-risk adult febrile neutropenia during cancer chemotherapy in the USA. Support Care Cancer 16(2):181â191, 2008.
2. Sipsas NV, Bodey GP, Kontoyiannis DP: Perspectives for the management of febrile neutropenic patients with cancer in the 21st century. Cancer 103(6):1103â1113, 2005.
3. National Comprehensive Cancer Network: Clinical Practice Guideline: Prevention and Treatment of Cancer-Related Infections. V.2.2009. Available at http://www.nccn.org/professionals/physician_gls/PDF/infections.pdf. Accessed on May 2, 2010.
4. Pizzo PA: Management of fever in patients with cancer and treatment-induced neutropenia. N Engl J Med 328(18):1323â1332, 1993.
5. DiNubile MJ: Fever and neutropenia: Still a challenge. Contemp Intern Med 7:35â37,41â35, 1995.
6. Wisplinghoff H, Seifert H, Wenzel RP, et al: Current trends in the epidemiology of nosocomial bloodstream infections in patients with hematological malignancies and solid neoplasms in hospitals in the United States. Clin Infect Dis 36(9):1103â1110, 2003.
7. Klastersky J, Paesmans M, Rubenstein EB, et al: The Multinational Association for Supportive Care in Cancer risk index: A multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol 18(16):3038â3051, 2000.
8. Gaur AH, Flynn PM, Giannini MA, et al: Difference in time to detection: A simple method to differentiate catheter-related from non-catheter-related bloodstream infection in immunocompromised pediatric patients. Clin Infect Dis 37(4):469â475, 2003.
9. O'Grady NP, Barie PS, Bartlett JG, et al: Guidelines for evaluation of new fever in critically ill adult patients: 2008 update from the American College of Critical Care Medicine and the Infectious Diseases Society of America. Crit Care Med 36(4):1330â1349, 2008. (See Erratum in: Crit Care Med 2008 Jun;36(6):1992.)
10. DuPont H, Sack RB, Tarr P, et al: Practice guidelines for the management of infectious diarrhea. Clin Infect Dis 32(3):331â351, 2001.
11. Valdivieso M, Gil-extremera B, Zornoza J, et al: Gram-negative bacillary pneumonia in the compromised host. Medicine (Baltimore) 56(3):241â254, 1977.
12. Maschmeyer G: Pneumonia in febrile neutropenic patients: Radiologic diagnosis. Curr Opin Oncol 13(4):229â235, 2001.
13. Hughes WT, Armstrong D, Bodey GP, et al: 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 34(6):730â751, 2002.
14. Wade JC: Management of infection in patients with acute leukemia. Hematol Oncol Clin North Am 7(1):293â315, 1993.
15. Yahav D, Paul M, Fraser A, et al: Efficacy and safety of cefepime: A systematic review and meta-analysis. Lancet Infect Dis 7(5):338â348, 2007.
16. Paul M, Yahav D, Fraser A, et al: Empirical antibiotic monotherapy for febrile neutropenia: Systematic review and meta-analysis of randomized controlled trials. J Antimicrob Chemother 57(2):176â189, 2006.
17. Flaherty JP, Waitley D, Edlin B, et al: Multicenter, randomized trial of ciprofloxacin plus azlocillin versus ceftazidime plus amikacin for empiric treatment of febrile neutropenic patients. Am J Med 87(5A):278Sâ282S, 1989.
18. Cometta A, Zinner S, de Bock R, et al: Piperacillin-tazobactam plus amikacin versus ceftazidime plus amikacin as empiric therapy for fever in granulocytopenic patients with cancer. The International Antimicrobial Therapy Cooperative Group of the European Organization for Research and Treatment of Cancer. Antimicrob Agents Chemother 39(2):445â452, 1995.
19. Cordonnier C, Herbrecht R, Pico JL, et al: Cefepime/amikacin versus ceftazidime/amikacin as empirical therapy for febrile episodes in neutropenic patients: A comparative study. The French Cefepime Study Group. Clin Infect Dis 24(1):41â51, 1997.
20. Siegel JD, Rhinehart E, Jackson M, et al: Management of multidrug-resistant organisms in health care settings, 2006. Am J Infect Control 35(10 suppl 2):S165âS193, 2007.
21. Siegel JD, Rhinehart E, Jackson M, et al: 2007 guideline for isolation precautions: Preventing transmission of infectious agents in health care settings. Am J Infect Control 35(10 suppl 2):S65âS164, 2007.
22. Dellinger RP, Levy MM, Carlet JM, et al: Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med 34(1):17â60, 2008.
23. Cronin L, Cook DJ, Carlet J, et al: Corticosteroid treatment for sepsis: A critical appraisal and meta-analysis of the literature. Crit Care Med 23(8):1430â1439, 1995.
24. Mermel LA, Allon M, Bouza E, et al: Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 49(1):1â45, 2009.
25. Hockenhull JC, Dwan KM, Smith GW, et al: The clinical effectiveness of central venous catheters treated with anti-infective agents in preventing catheter-related bloodstream infections: A systematic review. Crit Care Med 37(2): 702-712, 2009.
26. Casey AL, Mermel LA, Nightingale P, et al: Antimicrobial central venous catheters in adults: a systematic review and meta-analysis. Lancet Infect Dis 8:763-776, 2008.
27. Centers for Disease Control and Prevention: Guidelines for the Prevention of Intravascular Catheter-Related Infections. MMWR 51(RR-10):1-26, 2002.
28. Zitella L, Gobel BH, O'Leary C, et al: Prevention of Infection, in Eaton LH, Tipton JM (eds): Putting Evidence Into Practice: Improving Oncology Patient Outcomes, pp 267â283. Pittsburgh, PA, Oncology Nursing Society, 2009.
29. Centers for Disease Control and Prevention: Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008. Available at http://www.cdc.gov/ncidod/dhqp/pdf/guidelines/Disinfection_Nov_2008.pdf. Accessed on May 3, 2010.
30. Wilcox MH, Fawley WN: Hospital disinfectants and spore formation by Clostridium difficile. Lancet 356(9238):1324, 2000.
31. Aboelela SW, Saiman L, Stone P, et al: Effectiveness of barrier precautions and surveillance cultures to control transmission of multidrug-resistant organisms: A systematic review of the literature. Am J Infect Control 34(8):484â494, 2006.
32. Larson E: Skin hygiene and infection prevention: More of the same or different approaches? Clin Infect Dis 29(5):1287â1294, 1999.
33. Centers for Disease Control and Prevention: Guideline for Hand Hygiene in Health-Care Settings: Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR 51(RR-16):1â45, 2002.
34. Ayliffe GA, Babb JR, Davies JG, et al: Hand disinfection: A comparison of various agents in laboratory and ward studies. J Hosp Infect 11(3):226â243, 1988.
35. Kampf G, Kramer A: Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clin Microbiol Rev 17(4):863â893, 2004.
36. Oughton MT, Loo VG, Dendukuri N, et al: Hand hygiene with soap and water is superior to alcohol rub and antiseptic wipes for removal of Clostridium difficile. Infect Control Hosp Epidemiol 30(10):939â944, 2009.
37. Jabbar U, Leischner J, Kasper D, et al: Effectiveness of alcohol-based hand rubs for removal of Clostridium difficile spores from hands. Infect Control Hosp Epidemiol 31(6):565â570, 2010.
38. Pittet D, Allegranzi B, Boyce J: The world health organization guidelines on hand hygiene in health care and their consensus recommendations. Infect Control Hosp Epidemiol 30(7):611â622, 2009.
39. Gilbert DN, Moellering RC, Eliopoulos GM, et al (eds): The Sanford Guide to Antimicrobial Therapy, 40th ed. Sperryville, VA, Antimicrobial Therapy, Inc., 2010.