SABCS: Extending Tamoxifen Therapy for Breast Cancer Improves Survival
Patients who took tamoxifen as adjuvant therapy for ER-positive breast cancer for 10 years had both a reduced risk of recurrence and better overall survival compared to patients who stopped after 5 years, according to results of the ATLAS study presented at SABCS.
Patients who took tamoxifen for 10 years as adjuvant therapy for their estrogen receptor (ER)-positive breast cancer had both a reduced risk of recurrence and better overall survival compared to patients who stopped after 5 years, according to results of the ATLAS study presented at the San Antonio Breast Cancer Symposium (SABCS). The results were also published today in the Lancet. The greatest benefit to patients was seen in the second decade after their diagnosis, according to the authors of the study. The greatest benefit was seen 10 to 14 years after a patient’s initial diagnosis.
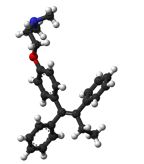
Ball-and-stick model of the tamoxifen molecule, as found in the solid state
According to presenter Christina Davies, MD, University of Oxford in the United Kingdom, while 5 years of tamoxifen provides an established benefit, reducing breast cancer mortality by almost one-third compared to no tamoxifen treatment, 10 years of tamoxifen appears to be even better. The ATLAS study shows that 10 years of the therapy decreases breast cancer mortality by one-half in the second decade after diagnosis, according to Davies.
The continuation of the ATLAS (Adjuvant Tamoxifen, Longer Against Shorter) study, funded by the Clinical Trial Service Unit and Epidemiological Studies Unit at the University of Oxford, England, enrolled 6,846 women who had ER-positive breast cancer between 1996 and 2005 and who were already taking tamoxifen for 5 years on the trial. About one-half of the patients had node-positive disease. One half of the patients were randomly assigned to an additional 5 years of tamoxifen and one-half were monitored without any further treatment.
While the recurrence and death rates were similar in the two study groups between years 5 and 9 of tamoxifen therapy, after year 10 women who continued tamoxifen for 10 years had a 25% lower rate of recurrence and a 29% lower breast cancer mortality compared to women who stopped tamoxifen after 5 years.
The study found that those women who took tamoxifen for 10 years had a 12.2% risk of death from breast cancer from years 5 to 14 after diagnosis compared to a 15% risk among those who took the drug for 5 years. Analysis of the trial starting at year 5 found that the risk of recurrence at year 15 was 21.4% in those participants who continued on tamoxifen compared to 25.1% for those who did not continue the treatment.
“Results from this trial are not surprising in the sense that hormone receptor–positive breast cancer continues to recur beyond the 5 years of treatment,” said Mothaffar Fahed Rimawi, MD, of the Baylor College of Medicine in Houston, Texas. “Actually almost half of breast cancer recurrences in this group occur beyond year 5, so it makes sense that longer treatment would be better.” Rimawi highlighted that previous smaller studies with 10-year tamoxifen treatment have had mixed results.
Compared to 2 years of adjuvant treatment, 5 years of tamoxifen was previously established as improving long-term survival and reducing the risk of recurrence, as well as reducing the risk of developing a new cancer in the patient’s opposite breast. Treatment of 5 years has been shown to reduce the risk of death from breast cancer not only during the treatment but for the first 15 years postdiagnosis.
However, the best duration of treatment and whether extending treatment would result in a further decrease in 15-year breast cancer mortality was still an important question, particularly as millions of women take adjuvant tamoxifen for their breast cancer. The ATLAS trial is the largest breast cancer trial to be undertaken. The study was started in the mid 1990s and accrued almost 13,000 women.
Tamoxifen is not without side effects, including a risk of endometrial cancer. However, because endometrial cancer is mostly curable and the mortality risk from this cancer is low, the benefit of preventing breast cancer recurrence outweighs the risk, said researchers. The excess risk of death from endometrial cancer was 0.2% by year 15 post-diagnosis (0.4% risk of death for those taking tamoxifen for 10 years compared to 0.2% for those taking tamoxifen for 5 years). No evidence of increased stroke risk during tamoxifen treatment was detected. “Overall the benefits of extended tamoxifen seemed to outweigh the risks substantially,” said Trevor J. Powles, PhD, of the Cancer Centre, London, in a commentary accompanying the study publication.
Even though the risk for endometrial cancer is increased, Rimawi believes this is a rare complication. “Moreover, I expect this study to potentially impact premenopausal women who are not at risk for endometrial carcinoma, since postmenopausal women are usually treated with aromatase inhibitors [as adjuvant therapy]. Therefore, I don't find this a deterrent.”
Compliance in this study was 80%. Thus, the benefits reported in this study could be even greater with a higher compliance. According to Powles, extending tamoxifen treatment to 10 years for premenopausal women could provide added benefit but that the course of treatment for postmenopausal women including length of optimal aromatase inhibitor and tamoxifen treatment for those with both a poor and less poor prognosis remains to be confirmed through further clinical trials.
“An important factor is that patients have to take these medicines for years and after a while, compliance drops,” said Rimawi. Tamoxifen can cause hot flashes and vaginal dryness, which can be well-managed medically but can be severe. More rare toxicities include blood clots and uterine cancer.
“I think the results of ATLAS will open the door for other studies about longer treatment with hormonal therapy,” said Rimawi. “Long-term treatment with hormonal therapy to keep tumors from recurring may become the norm over the next few years.” Currently, most menopausal women in the United States and other countries are given aromatase inhibitors for 5 years as adjuvant therapy. The question now becomes whether 10 years of tamoxifen should replace aromatase inhibitors in this patient population. Ongoing studies are addressing whether 5 or 10 years of aromatase inhibitors produces better outcomes.
For premenopausal women, 10 years of tamoxifen is a good option, said Rimawi, “especially for women at higher risk of recurrence.”