SABCS: Mixed Findings Fail to Clarify Role of Bisphosphonates
Results of 4 trials involving bisphosphonates in a range of protocols and patient cohorts suggest that the role of these agents in preventing recurrence of breast cancer remains to be defined. In 2 of the 4 studies reported, favorable outcomes were obtained following intravenous administration of zoledronic acid. Neither of two trials in which a bisphosphonate was administered orally, however, achieved its primary endpoint.
SAN ANTONIO-Results of 4 trials involving bisphosphonates in a range of protocols and patient cohorts suggest that the role of these agents in preventing recurrence of breast cancer remains to be defined. In 2 of the 4 studies reported, favorable outcomes were obtained following intravenous administration of zoledronic acid. Neither of two trials in which a bisphosphonate was administered orally, however, achieved its primary endpoint.
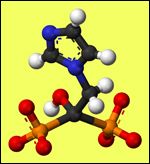
3D representation of zoledronic acid
ABCSG-12-Data from the Austrian Breast & Colorectal Cancer Study Group (ABCSG-12) confirmed and extended data reported at 48 months and 62 months of follow-up, reported Michael Gnant, MD, professor of surgery at the Medical University of Vienna. Now at 84 months of follow-up, patients are experiencing fewer recurrences of breast cancer and improved rates of survival with few toxic side effects (SABCS 2011 abstract S1-2).
"We have confirmed what this trial showed initially, which was both exciting and surprising," said Dr. Gnant. "The continued success of this treatment means we can intervene early and still observe persistence of the benefit of treatment."
In the 4-arm trial, researchers randomly assigned 1,803 premenopausal patients with early-stage, estrogen receptor (ER)-positive breast cancer to receive tamoxifen or anastrozole or each of these two treatments with zoledronic acid for three years. In the initial report, presented in 2008, Gnant and his colleagues reported significantly improved disease-free survival.
Long-term data at 84 months after treatment shows a 28% reduced risk for recurrence and a 36% reduction in risk for death among patients treated with zoledronic acid. There have been no reports of osteonecrosis of the jaw or renal failure.
Patients aged > 40 years with presumed complete ovarian blockade had a 34% reduced risk for recurrence and a 44% percent reduced risk for death. No significant survival benefits were observed among patients aged < 40 years.
These data, considered with previously demonstrated bone-protective effects of zoledronic acid, suggest that adding zoledronic acid to adjuvant endocrine therapy including ovarian function suppression should be considered for premenopausal women with ER-positive early breast cancer, said D. Gnant.
ZO-FAST: Long-term Outcomes-Post-hoc data from the ZO-FAST (Zometa-Femara Adjuvant Synergy Trial) show that immediate initiation of zoledronic acid with letrozole led to a 34% improvement in disease-free survival (DFS) at 5 years among postmenopausal women with hormone receptor–positive early breast cancer compared to delayed initiation of zoledronic acid. Findings were reported by Richard H. de Boer, MD, of Royal Melbourne Hospital, Victoria, Australia (SABCS 2011 abstract S1-3). ZO-FAST assessed the impact of zoledronic acid (Zometa) on aromatase inhibitor-associated bone loss after surgery for early breast cancer (SABCS 2010).
The new, long-term data confirm the beneficial effects on bone mineral density (BMD). An exploratory subgroup analysis based on menopausal status indicates that zoledronic acid confers the most benefit to women who are truly menopausal at diagnosis, Dr. de Boer reported.
The study involved 1,065 postmenopausal women with hormone receptor–positive early breast cancer with a bone mineral density T score of –2. In addition to receiving adjuvant endocrine therapy with 2.5 mg of letrozole (Femara) four times daily for 5 years, the women were randomized to receive 4 mg of zoledronic acid injected intravenously every 6 months either immediately or when their post-baseline T score dipped below –2 or they suffered a nontraumatic/asymptomatic fracture.
Exploratory analyses of the 670 women who were postmenopausal for more than 5 years or older than 60 years at study entry showed that immediate zoledronic acid treatment significantly improved DFS, with a hazard ratio of 0.63, and significantly prolonged overall survival, with a hazard ratio of 0.50, compared with the delayed treatment group.
The benefits observed in BMD continued over 5 years, with a net difference of 10% favoring the immediate zoledronic acid group, Dr. de Boer said. Findings of this study, together with those of other recent studies "support the hypothesis that the anticancer benefits of zoledronic acid may best be realized in a low-estrogen environment," Dr. de Boer concluded.
Three confirmed cases of osteonecrosis of the jaw occurred during the trial, all in the immediate group.
NSABP Protocol B-34-Disappointing findings were reported from B-34, a prospective, randomized, double-blind, phase III clinical trial of oral clodronate in patients with stage I, II, or III breast cancer (SABC 2011 abstract S2-3). The largest placebo-controlled study to date of an oral bisphosphonate in patients with early breast cancer, the trial failed to meet its primary end point of disease-free survival (DFS), reported Alexander H.G. Paterson, MD, professor in the departments of medicine and oncology at the University of Calgary, Alberta, Canada.
Secondary end points were incidence of skeletal metastases, overall survival (OS), relapse-free survival, incidence of non-skeletal metastases, and incidence of skeletal morbid events.
Slightly more than 75% percent of 3311 patients evaluated had pathologically negative axillary nodes, 64% percent were older than 50 years at entry, and 22% had estrogen receptor (ER)-negative or progesterone receptor (PR)-negative breast cancer.
Patients were randomly assigned to receive oral clodronate 1600mg daily for 3 years compared to placebo given alone or in addition to adjuvant chemotherapy or hormone therapy. Patients also underwent surgery (lumpectomies or mastectomies) and received radiation therapy and chemotherapy or hormonal therapy. Median follow-up for patients who were still alive was 7.6 years.
There were 598 patients who experienced disease events, defined as any cancer (either recurrent breast cancer or a new primary) or death (cancer related or otherwise): 286 in the clodronate group and 312 in the placebo group. The relative reduction of events in the clodronate group was about 9% compared with the placebo group.
"This reduction was smaller than had been hoped for and was not statistically significant," said Dr. Patterson. A relative reduction in mortality of 16% was observed in the clodronate group, as well as reductions of 23% and 26% in skeletal and nonskeletal metastases, respectively.
"Although clodronate appeared more favorable for all endpoints, only the comparisons of the distant metastasis-free interval and nonskeletal metastasis-free interval were statistically significant and favorable for the clodronate patients," said Dr. Paterson.
Results also suggested that clodronate might perform better in patients who are 50 years or older when diagnosed with breast cancer, and in women with ER/PR-positive nodes. Clodronate was generally tolerable, and the toxicities observed were considered by the investigators mainly due to concomitant systemic chemotherapy.
GAIN Trial-Results from the prospective, multicenter, controlled, non-blinded, randomized phase 3 German Adjuvant Intergroup Node Positive (GAIN) study demonstrated no improvement in DFS among patients with breast cancer who were treated with dose-dense chemotherapy and the oral bisphosphonate ibandronate (2011 SABC abstract S2-4). Findings were reported by Volker Mbus, PhD, head of the department of obstetrics and gynecology at Klinikum Frankfurt Hchst GmbH, Frankfurt.
Investigators randomly assigned 3,023 patients with primary breast cancer to 2 different chemotherapy regimens and then further assigned them to 50 mg daily of oral ibandronate or observation. After a median follow-up of 38.7 months, "we found no significant difference between groups in the primary end point" of DFS, said Dr Mbus.
He described the results as "disappointing" compared to other studies of bisphosphonates in breast cancer patients. "So far, clinical trials of adjuvant bisphosphonates in early breast cancer have shown variable results, independent from their application (oral compared with intravenous)," he explained. "In the AZURE trial, 95% of patients received chemotherapy and only postmenopausal patients showed an improvement in the zoledronic acid group. "In our [GAIN] trial, all patients received dose-dense chemotherapy, and unfortunately, we could not show a benefit in any subgroup. We speculate that the high efficacy of dose-dense chemotherapy erases the potential effect of bisphosphonates, which is shown in patients with endocrine treatment only."
"There were four presentations on bisphosphonate therapy, and unfortunately, one is more puzzled than ever," commented Harold J. Burstein, MD, PhD, assistant professor of medicine at Harvard Medical School and medical oncologist in the Breast Oncology Center at Dana-Farber Cancer Institute, Boston. "The two largest studies showed no compelling gains; the two smaller studies suggested more benefit. It will take more analyses to help us understand whether or how to use these drugs to prevent breast cancer recurrence."
Gedatolisib Combo With/Without Palbociclib May Be New SOC in PIK3CA Wild-Type Breast Cancer
December 21st 2025“VIKTORIA-1 is the first study to demonstrate a statistically significant and clinically meaningful improvement in PFS with PAM inhibition in patients with PIK3CA wild-type disease, all of whom received prior CDK4/6 inhibition,” said Barbara Pistilli, MD.