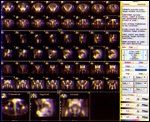
FIGURE 1
A 72-Year-Old Man With Prostate Cancer
The patient, L.E., is a 72-year-old white male who has been under our care for 10 years. He initially presented to our clinic in 1992, with a diagnosis of localized prostate cancer.
SECOND OPINION
Multidisciplinary Consultations on Challenging Cases
The University of Colorado Health Sciences Center holds weekly second opinion conferences focusing on cancer cases that represent most major cancer sites. Patients seen for second opinions are evaluated by an oncologist. Their history, pathology, and radiographs are reviewed during the multidisciplinary conference, and then specific recommendations are made. These cases are usually challenging, and these conferences provide an outstanding educational opportunity for staff, fellows, and residents in training.
The second opinion conferences include actual cases from genitourinary, lung, melanoma, breast, neurosurgery, and medical oncology. On an occasional basis, ONCOLOGY will publish the more interesting case discussions and the resultant recommendations. We would appreciate your feedback; please contact us at second.opinion@uchsc.edu.
E. David Crawford, MD
Professor of Surgery and Radiation Oncology
University of Colorado Health Sciences Center
Univeristy of Colorado Cancer Center Denver, Colorado
The patient, L.E., is a 72-year-old white male who has been under our care for 10 years. He initially presented to our clinic in 1992, with a diagnosis of localized prostate cancer.
History
In 1990, the patient had requested that his health-care provider screen him for prostate cancer. Citing the lack of data to support the value of early detection in prostate cancer, that physician had discouraged him from being screened. In 1991, he participated in a local health fair, where he had his prostate-specific antigen (PSA) level tested. Several weeks later, he learned that his PSA level was elevated at 13 ng/mL. His digital rectal exam was normal. Sextant biopsies were performed, revealing a Gleason 4+3, sum 7 in two of six biopsies.
The Gleason sum is an important pathologic scoring system. The most prevalent grade and second most prevalent grade of tumor on the needle biopsy are added together to achieve a Gleason sum. The lowest sum is 2 and the highest is 10. Sums 2-6 are considered low grade; 7 is intermediate; and 8-10 are high-grade cancers.
The patient was in good health and oversaw the activities on a ranch in southern Colorado. He related a past smoking history and moderate alcohol intake. He had no history of any cardiac or pulmonary disease. His father died of prostate cancer at age 93. Bone scans and pelvic computed tomography scans were normal at that time.
He was counseled as to treatment options, and it was recommended that he undergo either a radical prostatectomy or external-beam radiation. During the early 1990s, cryotherapy for prostate cancer was very popular. One patient advocate group strongly recommended this treatment option. There were claims of superior response and less morbidity then either of the two recommendations made to the patient. Despite the fact that this treatment was not covered by his health-care insurance, the patient chose cryotherapy.
Postoperative Course
In June 1992, the patient underwent cryotherapy for his prostate cancer. His postoperative course was complicated in that he was urinating flecks of tissue and had two episodes of urinary retention, necessitating placement of a Foley catheter. He maintained his potency for 3 months and then experienced the gradual onset of erectile dysfunction. At 18 months posttherapy, his PSA was
0.3 ng/mL.
In 1995, he was diagnosed with colon cancer and treated with a partial colectomy. Pathology revealed a Duke’s class C carcinoma of the colon. He was treated with adjuvant chemotherapy consisting of fluorouracil (5-FU) plus levamisole (Ergamisol). At the present time, he is considered to be disease-free.

Posttreatment Biopsy
Because of persistent erectile dysfunction and lack of response to sildenafil (Viagra) and alprostadil injections, a penile prosthesis was inserted. Both he and his partner were very satisfied with the results.
Over the past 3 years, his PSA has begun to rise. In April 2000, when his PSA level reached 3.1 ng/mL, prostate biopsies were obtained in an attempt to document a local recurrence (Figure 1). No evidence of malignancy was found. The patient did not have a follow-up until October 2001, when his PSA level was 5.4 ng/mL. He had no new complaints, but was concerned about the implications of the rising PSA. He stated that he wanted us to keep him alive for at least another 10 years.
Physical Exam
The physical examination revealed a healthy 72-year-old male. A penile prosthesis was in place, and the digital rectal exam showed a 25-g small fibrotic prostate with no nodularity. For this conference, a bone scan and ProstaScint scan were obtained.
Discussion
In summary, we have a healthy 72-year-old male diagnosed with prostate cancer in 1991. He was treated with a nontraditional therapy-cryotherapy-and has done reasonably well, with the exception of biochemical failure. The patient is quite concerned about the implications of the rising PSA blood test.
Biopsy Accuracy
FIGURE 2

Bone Scan
Dr. Michael Glode: Dr. Lucia, what is your feeling about the difference, if any, between Gleason patterns 4+3 vs 3+4?
Dr. Scott Lucia: Data from the Stanford and Wayne State groups show that the greater the volume of a high-grade component (Gleason grade 4 or 5), the worse the prognosis. Thus, disease-free survival following prostatectomy is lower for 4+3 tumors compared to 3+4 tumors at 5 years. These data are for prostatectomy specimens; it is not clear that this holds for biopsies. D’Amico in 1999 reported that 5-year PSA failure-free survival was significantly lower in patients whose biopsy scores were 4+3 vs 3+4. However, sampling is a major problem with needle biopsies. Therefore, the difference between a 3+4 and 4+3 biopsy may be more of a sampling issue than a truly prognostic one.
Dr. Andrew Kraft: How accurate are biopsies in determining the presence of prostate cancer in a gland following radiation therapy, or in this case, cryotherapy?
Dr. Lucia: Certainly if tumor is present we can diagnose it on biopsy. However, although I still grade tumors following radiation therapy, some feel that Gleason grading can be inaccurate following therapy. There can be sampling errors by which persistent cancer is missed.
Local vs Distant Recurrence
FIGURE 3
ProstaScint Scan
Dr. Marcus Chen: The patient’s bone scan has a small linear focus of increased activity involving the left anterior pubic ramus, which is not suspicious for metastases (Figure 2). There are no other areas of focal increased uptake. The ProstaScint scan demonstrates activity in the region of the prostatic bed, suspicious for prostate cancer recurrence (Figure 3). There is no focal increased activity in the pelvic lymph nodes.
Dr. E. David Crawford: Biochemical failure is the most common presentation for advanced prostate cancer. To me, and I believe to patients, advanced is synonymous with incurable. In many patients with biochemical failure there is a risk of dying "of" rather than "with" prostate cancer. In a manuscript published 3 years ago, we labeled this stage D1.5. (This refers to a rising PSA after failed local therapy.) Less than a decade ago, most patients with advanced prostate cancer presented with bone metastasis stage D2 (Tx, Nx, M+). Early-detection efforts have changed this pattern. A great deal of controversy exists regarding treatment for stage D1.5. Unfortunately, we don’t have any randomized clinical trials to address this issue.
In evaluating these patients, I ask two important questions: First, was this patient curable when initially diagnosed? And second, does this represent a local recurrence, a distant recurrence, or a combination of both?
A patient with an initial Gleason sum of 5, a PSA of 6 ng/mL, and a normal rectal exam (T1C) should be curable with local modalities. A patient with an initial Gleason sum of 8, PSA of 32 ng/mL, and a rock hard prostate is not going to be cured with local therapies such as radical prostatectomy or radiation therapy alone. This patient is in a gray zone. If we look up his chance of failing in well-publicized tables or artificial neural networks, again he is in a gray zone.
Using our artificial neural network programs (http://www.annsincap.org or www.prostatecalculator.org), which provide a method of analyzing multiple variables, he has a 57.3% chance of having extracapsular disease, an 84% 5-year chance of having a now rising PSA (undetectable) and a 76% chance at 10 years, all based on radical prostatectomy figures. Our current radiographic staging would suggest that this is a local rather than a distant recurrence.
Another factor in the patient’s history that favors a local rather than a distant recurrence is the fact that his PSA fell to a low level and gradually rose only in the past couple of years. Men who fail to reduce their PSA to negligible levels or have a rise in the first 18 months of therapy are more likely to have distant disease. A third factor favoring local disease is the slow doubling time of the PSA.
Value of Rebiopsy
Dr. David Raben: In light of Dr. Lucia’s previous comments, should we recommend a rebiopsy of his prostate?
Dr. Crawford: We could recommend a rebiopsy, but what if it were again negative? Does that mean that it is not a local recurrence? The biopsy would help us if positive but not if it were negative; as already stated, a negative biopsy could be the result of a sampling error. That said, if I were going to perform a salvage prostatectomy, I would like to have a biopsy-proven local recurrence.
Dr. Glode: So are we going to recommend rebiopsy?
Dr. Crawford: When I suspect that the patient has a local recurrence after radiotherapy, or in this case cryotherapy, I tell him we should proceed with a thorough work-up including a biopsy, only if they are going to consider a potentially curative salvage procedure such as prostatectomy, cryotherapy, or brachytherapy. This patient desires to be cured or at least to extend his life. He is concerned about his PSA rise. We all know that PSA is the abbreviation for prostate-specific antigen, but in this case it could also stand for "patient-stimulated anxiety." A decrease in his PSA would be viewed as a favorable response in the patient’s mind.
Role of Radiation Therapy
Dr. Crawford: So let’s assume that he undergoes a biopsy, which shows a Gleason 7 cancer in a biopsy. What do we recommend? Dr. Raben, what is the role of radiation therapy as a salvage procedure in this man?
Dr. Raben: No one institution has a vast experience of treating men failing cryotherapy with external-beam therapy. We have treated just two such patients in the past 5 years. The treatment was well tolerated, and one patient has had his PSA decrease to undetectable levels and remain there for 3 years.
Dr. Kraft: What is the role of radiation therapy in a patient failing radical prostatectomy?
Dr. Raben: That would be a lengthy discussion. The short answer is that there is a role in men who likely have a local recurrence. The key is to select patients who fail more than 1 year after surgery and have a PSA level of less than 2.0 ng/mL. In the most optimistic sense, there is an 80% response rate. Durable response depends on patient selection and varies from 20% to 50%.
Dr. Glode: Is there any role for brachytherapy in men failing external-beam therapy? I have seen two such men who have had brachytherapy after failing external-beam treatment, and they are both miserable. One required a colostomy because of a fistula and the other has severe irritative voiding symptoms.
Dr. Raben: Were they cured?
Dr. Glode: One was and one wasn’t.
Dr. Raben: I would not recommend this treatment because of the morbidity patients experience after external-beam treatment.
Salvage Prostatectomy
Dr. Kraft: What about a salvage prostatectomy?
Dr. Crawford: Candidates for salvage prostatectomy are men who were candidates for cure with surgery to begin with, chose another therapy, and failed. The failure needs to be detected early, as in this patient. I feel they should have a 10-year life expectancy, and I believe this patient does have a 10-year life expectancy. Having performed a number of salvage prostatectomies, my experience is that the procedure is associated with nearly a 100% impotency rate and around a 20% chance of severe urinary incontinence. Since this patient did not choose a radical prostatectomy as his initial treatment, I doubt he would consider it now.
Another option would be to repeat the cryotherapy. The instrumentation and techniques have substantially improved in the past decade. I have discussed this case with several of my colleagues experienced in cryotherapy; they claim this is an option and that the side effects are minimal.
Hormonal Therapy
Dr. Marshal Freeman: What is the role of hormonal therapy with and without chemotherapy in this patient?
Dr. Glode: To paraphrase Dr. Raben’s comments regarding adjuvant radiation, almost any form of hormonal therapy will lower his PSA and delay progression, but we have no proof that any form will increase his survival. There are no randomized trials to address this issue. This is unfortunate; most oncologists feel that hormonal therapy cannot cure prostate cancer. However, this belief is based on experience with advanced metastatic disease. The real question is, when hormonal therapy is employed earlier in the disease, could survival be improved?
A randomized trial that contained similar patients examined early long-term hormonal therapy vs delayed treatment in men found to have positive lymph nodes after a radical prostatectomy. The result of this trial was that only 5% of men receiving the immediate hormonal therapy died of prostate cancer vs nearly 30% who died in the delayed-treatment arm. These study patients may have had a lesser tumor burden at the time of entry than patients with rising PSAs. All patients had undergone radical prostatectomy, which historically leaves most men with an undetectable PSA for a while after surgery.
That said, there was a significant benefit to early hormonal therapy, and we could draw a parallel here for this patient.
Chemotherapy is generally reserved for hormone-refractory prostate cancer. In other tumor sites such as breast and colorectal cancer, it is more effective when used earlier in the disease. Perhaps the same is true for prostate cancer, but we don’t know. I would only recommend chemotherapy in the context of a clinical trial. Dr. Crawford, I know you have done some studies with hormonal therapy in rising PSAs; would you comment?
Dr. Crawford: In concert with Dr. Judd Moul at Walter Reed Army Medical Center, we just completed a large phase II study involving 73 patients with a rising PSA after failed local therapy. The drugs utilized were flutamide (Eulexin), 125 mg bid, and finasteride (Proscar), 5 mg bid. We instituted this study based on the synergistic interactions of these agents, their potency-sparing potential, and the lack of side effects generally associated with hormonal therapy.
The results are encouraging; nearly 60% of patients developed an undetectable PSA. Among patients in whom therapy was instituted before the PSA reached a level of 5 ng/mL, 95% achieved an undetectable level. The longest time on study has been 8 years. All of the patients who failed this regimen responded to hormonal therapy with luteinizing hormone-releasing hormone (LHRH) agonists, with or without an antiandrogen. Potency was preserved in potent patients. The major side effect was gynecomastia.
I am encouraged by these results and feel that a phase III study is indicated. This approach fits the definition of "step-up" therapy-ie, when a lesser therapy, for example, finasteride and flutamide, is followed by a more aggressive therapy, such as an LHRH agonist.
Formulating a Recommendation
Let’s summarize and make a recommendation. This is a difficult case, and as we have heard, many controversies exist regarding intervention. I believe the options presented are to do nothing, administer some local therapy, or give a form of hormone therapy.
Dr. Raben: I would offer the patient definitive radiation therapy.
Dr. Glode: I would favor some form of local therapy, assuming this is a local recurrence. My preference would be radiation therapy. A second option would be hormonal therapy.
Dr. Craig Berman: Observation is certainly an option, with therapy to be instituted when the PSA reaches a certain level.
Dr. Crawford: I agree, but when do we pull the trigger and treat the patient? A series of radical prostatectomy failures revealed that the average time to metastatic disease was 8 years, with death at 13 years. I am not sure this approach is appropriate for this patient. The study I mentioned involved a select group of patients. I believe that the outcome is predicated on many factors, including initial PSA, Gleason score, age of the patient, clinical stage, and type of treatment.
I know this patient, and he would not accept observation. Right or wrong, this patient wants treatment. He wants to see his PSA fall. His quality of life is altered by his PSA rise. He knows the data point to a local recurrence. I would favor either repeat cryotherapy or radiation therapy. Unfortunately we don’t have a lot of experience with either one. Step-up hormonal therapy would be a close second option for this patient.
Dr. Crawford: Any other comments?
Dr. Frances Crighton: If we recommend hormonal therapy with an LHRH agonist, should it be for life, intermittent, or for a set period such as 3 years?
Dr. Glode: Good question, we don’t know the answer to that question. There is a clinical trial by the Southwest Oncology Group examining continuous and intermittent therapy in patients with advanced disease. There is also a Canadian trial comparing these therapies in patients with rising PSA after failing radiation therapy. We don’t know the results of either of these studies. My opinion is that intermittent therapy is experimental, and patients should only be treated in a clinical trial; if the patient chooses hormonal therapy, it should be lifelong.
Dr. Crawford: Therefore, our recommendations to this patient are for a prostate biopsy and some form of local therapy. The majority of the second opinion team favors radiation therapy, although repeat cryotherapy is an option. The second option would be hormonal therapy.
FIGURE 4
Second Opinion Biopsy
Dr. Lucia: What would you recommend if the biopsies were negative?
Dr. Glode: I believe the biopsy should be performed more for academic reasons, and I would not change my recommendations.
Second Opinion Recommendations
1. Prostate biopsy, and then consider a local therapy-either radiation therapy or repeat cryotherapy.
2. Hormonal therapy.
Case Outcome
Based on the decision of this second opinion conference, another biopsy was performed in November 2001 (Figure 4). A total of seven cores were obtained, and assessment revealed a Gleason pattern 3+4 cancer involving most of three of five cores from the right and one of two cores from the left prostate. There was no perineural invasion or evidence of capsular penetration. The patient has chosen radiation therapy.
References:
Benson RC: Total androgen blockade: The United States experience. Eur Urol 24S:72-76, 1993.
Bolla M, Gonzalez D, Warde P, et al: Improved survival in patients with locally advanced prostate cancer treated with radiotherapy and goserelin. N Engl J Med 337:295-300, 1997.
Crawford ED, Blumenstein B: Proposed substages for metastatic prostate cancer. Urology 50:1027-1028, 1998.
Crawford ED, Eisenberger M, McLeod DG, et al: A controlled trial of leuprolide with and without flutamide in prostatic carcinoma. N Engl J Med 321:419-424, 1989.
Messing EM, Manola J, Sarosdy M, et al: Immediate hormonal therapy compared with observation after radical prostatectomy and pelvic lymphadenectomy in men with node-positive prostate cancer. N Engl J Med 41:1781-1788, 1999.
Pilepich MV et al: Phase III Radiation Therapy Oncology Group trial 8610 of androgen deprivation adjuvant to definitive radiotherapy in selected locally advanced carcinoma of the prostate. Presented at the 42nd Annual Meeting of the American Society for Therapeutic Radiology and Oncology, 2000.
Pilepich MV, Krall JM, al-Sarraf M, et al: Androgen deprivation with radiation therapy compared with radiation therapy alone for locally advanced prostatic carcinoma: A randomized comparative trial of the Radiation Therapy Oncology Group. Urology 45:616-623, 1995.