ACOG Recommends Salpingectomy for Ovarian Cancer Prevention
ACOG recently released a Committee Opinion on the use of salpingectomy for ovarian cancer prevention in at-risk women undergoing routine pelvic surgery.
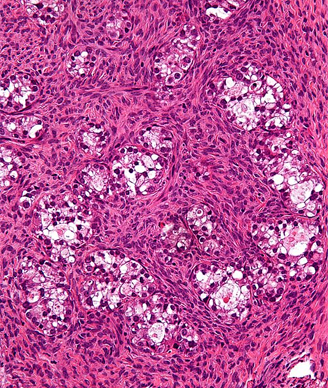
High magnification micrograph of an ovarian clear cell carcinoma. Copyright 2011 Nephron.
The American College of Obstetricians and Gynecologists (ACOG) recently released a Committee Opinion on the use of salpingectomy for ovarian cancer prevention in women with population risk already undergoing routine pelvic surgery for benign disease. The opinion was published in the January issue of Obstetrics & Gynecology.
According to the opinion, evidence has shown that serous, endometrioid and clear cell carcinomas may be derived from the fallopian tube and endometrium, and not from the ovary.
“In women with a genetic predisposition for ovarian cancer, lesions have been found in the fallopian tubes that closely resemble ovarian high-grade serous carcinomas or serous tubal intraepithelial carcinomas,” wrote the committee on Gynecologic Practice. “These lesions are thought to be the primary source of ovarian carcinoma that secondarily involves the ovary.”
Based on this, ACOG recommended that a surgeon and patient discuss the potential benefits of the removal of the fallopian tubes during a hysterectomy in women at population risk of ovarian cancer who are not having an oophorectomy, mainly that prophylactic salpingectomy may prevent ovarian cancer. However, the committee recommended more randomized clinical trials to support the validity of this approach as a method to reduce ovarian cancer incidence.
In addition to possible benefits, “salpingectomy at the time of hysterectomy or as a means of tubal sterilization appears to be safe, without an increase in complications, such as the need for blood transfusions and readmissions, compared with hysterectomy alone or tubal ligation,” the committee wrote.
The discussion of risk and benefit between the physician and patient should include an informed consent discussion about the role of oophorectomy and bilateral salpingo-oophorectomy. In addition, when counseling a patient about bilateral salpingectomy, clinicians should mention that the procedure provides women with an effective method of contraception.
“Although there is no information about the effectiveness of complete salpingectomy as a method of sterilization, possible surrogates may include postpartum partial salpingectomy and interval partial salpingectomy, which were found to have 7.5 and 20.1 cumulative probability of pregnancy per 1,000 procedures, respectively, in the US Collaborative Review of Sterilization study,” the committee wrote.
Finally, the committee pointed out that the physician’s approach to a hysterectomy or sterilization should not be altered or influenced by the possible benefits of salpingectomy. Instead, surgeons should continue to observe and practice minimally invasive procedures.