Active Monitoring Noninferior to Standard Surgery, RT in Low-risk DCIS
Active monitoring had similar rates of invasive cancer in the ipsilateral breast as guideline concordant care for the low-risk DCIS population.
Active monitoring had similar rates of invasive cancer in the ipsilateral breast as guideline concordant care for the low-risk DCIS population.
Active monitoring (AM) in patients with low-risk ductal carcinoma in situ (DCIS) demonstrated a noninferior invasive cancer in the ipsilateral breast rate compared with those who were randomized to guideline concordant care (GCC) of surgery and potentially radiation, according to findings from the COMET trial (NCT02926911) that were presented during the 2024 San Antonio Breast Cancer Symposium and simultaneously published in JAMA.1,2
Results showed that the 2-year ipsilateral invasive cancer rate, which was the study’s primary end point, was 5.9% (95% CI, 3.71-8.04) in the GCC arm compared with 4.2% (95% CI, 2.31-6.00) of patients who underwent AM, leading to a 1.7% difference.
“There were no significant differences between groups in invasive tumor size, node status, or tumor grade,” lead study author E. Shelley Hwang, MD, MPH, Mary and Deryl Hart Distinguished Professor of Surgery in the School of Medicine, professor of surgery vice-chair of research in the Department of Surgery, professor of radiology, within Duke University School of Medicine, said in a press conference during the meeting. “We found no obvious imbalance in patient characteristics between groups, but cannot exclude introduction of bias.”
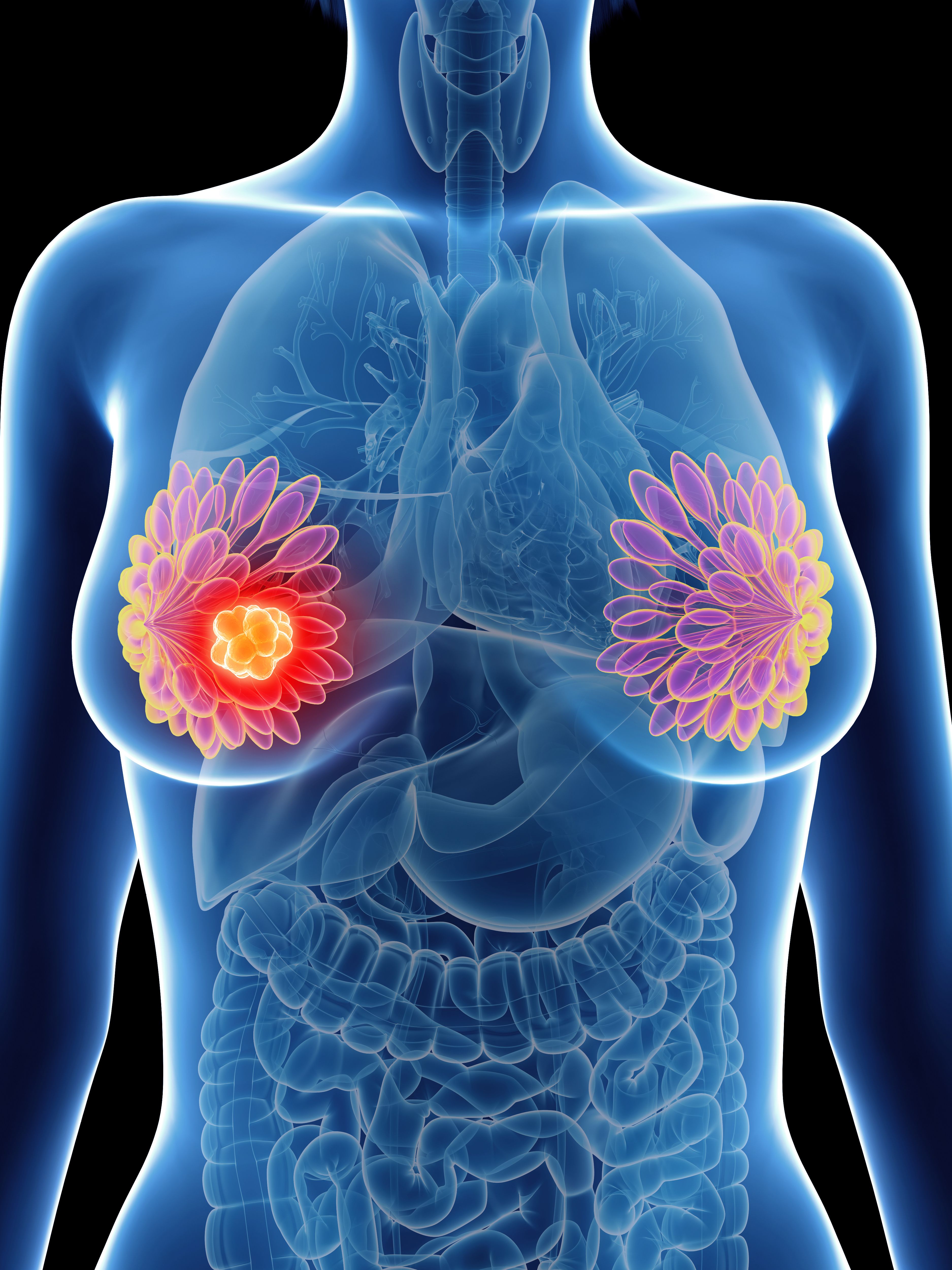
A precancer and preinvasive cancer, DCIS can, but does not always progress to invasive cancer, with an estimated annual incidence of more than 50,000 cases. Standard treatment comprises surgical excision with or without radiotherapy as a method to prevent disease progression.
In the prospective, noninferiority COMET trial, investigators randomized patients 1:1 to receive GCC of breast-conserving surgery or mastectomy at diagnosis, with adjuvant radiation therapy per recommendation from a radiation oncologist (n = 498) or AM with ipsilateral mammogram every 6 months, a biopsy for imaging changes, and GCC upon diagnosis of invasive breast cancer (n = 497). Adjuvant endocrine therapy (ET) was permitted in both arms.
To be eligible for enrollment, female patients had to be at least 40 years old with a new diagnosis of grade 1/2 hormone receptor–positive DCIS without invasive disease, and 2 biopsies if the extent of disease is greater than 4 cm.
Overall, the primary end point was 2-year cumulative rate of ipsilateral invasive breast cancer at any time following randomization. In the GCC arm, the primary outcome was detection of any IBC at time of surgery (upstaging) or recurrence; in the AM arm, this was also any IBC detected on core needle biopsy during monitoring, or at time of surgery (upstaging).
Invasive cancer diagnosis was evaluated by randomized group, which served as a secondary end point.
Here, the mean IBC size was 0.78 cm (SD, 1.08) in the GCC arm (n = 27; 58.7%) and was 0.94 cm (SD, 0.77) in the AM arm (P = .33); the median IBC size was 0.4 cm (IQR, 0.28-0.9) and 0.85 cm (IQR, 0.2-1.63).
Between the GCC and AM arms, IBC ERBB2 status was 0 (33.3% vs 31.6%, respectively; P = .67), 1+ (22.2% vs 42.1%), 2+ (14.8% vs 21.1%), and 3+ (3.7% vs 0%). Node status at sentinel lymph node biopsy was 0 (29.6% vs 42.1%; P = .41). 1+ (18.5% vs 10.5%), and not performed/unknown (51.9% vs 47.4%). The IBC grade was high (3.7% vs 15.8%; P = .34), intermediate (40.7% vs 31.6%), or low (37.0% vs 21.1%).
Investigators also analyzed treatments received by randomized group. There were 473 patients who received the 2-year cumulative treatment (49.4%) in the GCC arm compared with 484 patients in the AM arm (50.6%).A total 65.5% and 71.3% of patients, respectively, received endocrine therapy, 26.6% and 7.4% received radiation, and 1.1% and 1.2% received chemotherapy.
Regarding surgery, 48.2% underwent lumpectomy on the GCC arm vs 13.2% on the AM arm; for mastectomy, these rates were 5.5% and 3.7%, and was 2.1% and 0% with reexcision. The overall non-acceptance of allocation rate was 29.7%.
The 2-year ipsilateral invasive cancer rate was also tested in a per protocol analysis. Here, these rates were 8.7% (95% CI, 5.06-12.21) in the GCC arm vs 3.1% (95% CI, 2.31-6.00), leading to a 5.6% difference.
Investigators also conducted an as-treated analysis, as some patients did not accept their arm allocation. Overall (n = 46), the median IBC size was 0.45 cm (95% CI, 0.23-1.1), the node status at sentinel lymph node biopsy (SLNB) was 0% (34.8%), 1+ (15.2%), and not performed/unknown (50.0%); 8.7% of patients had high-grade IBC.
In patients assigned to GCC and remained on the GCC arm (n = 21; 45.7%), the median IBC size was 0.4 cm (95% CI, 0.3-0.9), the node status at SLNB was 0% (28.6%), 1+ (14.3%), and not performed/unknown (57.1%); 4.8% of patients had high-grade IBC.
For patients who were assigned to AM and stayed on AM (n = 12; 26.1%), the median IBC size was 1.4 cm (95% CI, 0.8-1.7), the node status at SLNB was 0% (41.7%), 1+ (8.3%), and not performed/unknown (50.0%); 16.7% of patients had high-grade IBC.
For patients who were assigned to GCC and were allocated to AM (n = 6; 13%), the median IBC size was 0.48 cm (95% CI, 0.15-2.85), the node status at SLNB was 0% (33.3%), 1+ (33.3%), and not performed/unknown (33.3%); no patients had high-grade IBC.
Across these cohorts, the P values for IBC median size was 0.17, 0.85 for node status on SLNB, and 0.78 for IBC highest grade.
Hwang concluded that while these short-term results are encouraging, additional follow-up will identify the long-term outcomes of active monitoring.
Disclosures: Hwang cited consulting roles with Merck; advisory board roles with Clinetic, Exai Bio, and Havah Therapeutics; and research support from PCORI, National Institute of Health, DOD, and Breast Cancer Research Foundation.
References
- Hwang ES, Hyslop T, Lynch T, et al. Early oncologic outcomes following active monitoring or surgery (+/- radiation) for low risk DCIS: the comparing an operation to monitoring, with or without endocrine therapy (COMET) study (AFT-25). Presented at: 2024 San Antonio Breast Cancer Symposium; December 10-13, 2024; San Antonio, TX. Abstract GS2-05.
- Hwang ES, Hyslop T, Lynch T, et al. Active monitoring with or without endocrine therapy for low-risk ductal carcinoma in situ: the COMET randomized clinical trial. JAMA. Published online December 12, 2024. doi:10.1001/jama.2024.26698
Gedatolisib Combo With/Without Palbociclib May Be New SOC in PIK3CA Wild-Type Breast Cancer
December 21st 2025“VIKTORIA-1 is the first study to demonstrate a statistically significant and clinically meaningful improvement in PFS with PAM inhibition in patients with PIK3CA wild-type disease, all of whom received prior CDK4/6 inhibition,” said Barbara Pistilli, MD.