Afatinib Delayed Progression of Recurrent Head and Neck Cancer
In patients with recurrent or metastatic head and neck squamous cell carcinoma, afatinib better delayed cancer progression compared with methotrexate, according to results presented at the 2014 ESMO Congress.
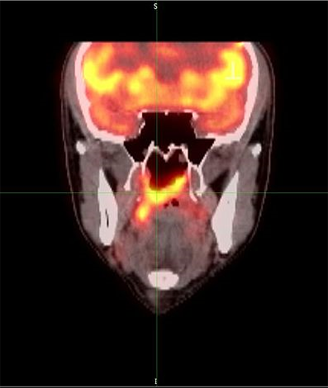
PET Scan of nasopharynx carcinoma; source: Sanko, Wikimedia Commons
The ErbB family blocker afatinib better delayed progression and deterioration of patient-reported outcomes in patients with recurrent or metastatic head and neck squamous cell carcinoma than did treatment with methotrexate, according to primary efficacy results of the Lux-Head & Neck 1 trial.
Specifically, patients treated with afatinib had a delayed worsening of symptoms, including pain and swallowing compared to patients treated with chemotherapy. Afatinib is the first tyrosine kinase inhibitor to demonstrate a significant benefit in patients with head and neck squamous cell carcinoma, according to Jean-Pascal Machiels, MD, a medical oncologist at Cliniques Universitaires St. Luc, in Brussels, Belgium, who presented the results of the Lux-Head & Neck 1 trial (Abstract 29LBA_PR), at the European Society for Medical Oncology (ESMO) 2014 Congress.
The phase III study randomly assigned patients with recurrent and/or metastatic head and neck squamous cell carcinoma to treatment with 40 mg per day afatinib (n = 322) or 40 mg/m2 per week intravenous methotrexate (n = 161).
Patients assigned to afatinib had a significant improvement in progression-free survival compared with those assigned methotrexate (2.6 months vs 1.7 months; HR = 0.80; 95% CI, 0.65-0.98; P = .03). In addition, treatment with afatinib was associated with a higher rate of disease control compared with methotrexate (49.1% vs 38.5%; P = .04).
However, the researchers found no significant difference between the two treatments for overall survival (6.8 months vs 6.2 months) or overall response rate (10.2% vs 5.6%).
“Many potential reasons could explain why we were not able to demonstrate a survival benefit,” Machiels said in a prepared statement. “It could be simply because afatinib does not improve survival. However, 50% of the patients in both arms received subsequent therapies that could have influenced the survival benefit, for example a significant number of patients received subsequent anti-EGFR therapies in the methotrexate arm.”
The study was designed to look at differences in patient-reported outcomes. Data showed that treatment with afatinib delayed deterioration of global health status, pain, and swallowing compared with methotrexate (P < .03 for all). Afatinib was also associated with an improvement in reported pain (P = .03).
Rash/acne and diarrhea were the most commonly reported grade 3/4 drug-related adverse events reported in patients treated with afatinib. However, patients assigned afatinib had fewer treatment-related dose reductions, discontinuations, and fatal events.
Moving forward, Machiels hopes to focus research on identifying which patients will derive the most benefit from treatment with afatinib.