AI Model May Predict Toxicity Risk in Breast Cancer Surgery Populations
Investigators will assess the PRE-ACT tool’s ability to predict adverse effects such as skin and heart damage in a phase 3 trial.
“Patients identified at higher risk of arm swelling could be offered additional supportive measures, such as wearing an arm compression sleeve during treatment, which has been shown to reduce arm swelling in the long term,” according to Tim Rattay, a consultant breast surgeon and associate professor at the Leicester Cancer Research Centre of the University of Leicester.
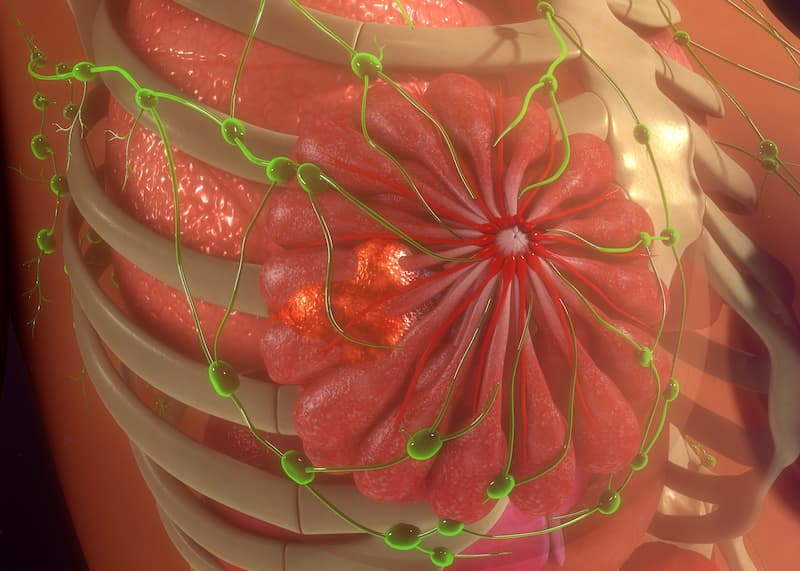
The use of an artificial intelligence (AI)–based tool may be able to predict adverse effects (AEs) including lymphedema in patients with breast cancer who undergo surgery or radiotherapy, according to findings presented at the 14th European Breast Cancer Conference.1
As part of the Prediction of Radiotherapy Side Effects Using Explainable AI for Patient Communication and Treatment Modification (PRE-ACT) project, investigators assessed outcomes in 6361 patients with breast cancer to train learning algorithms to help forecast arm swelling for up to 3 years following radiotherapy or surgery.Across 3 datasets, 6% of patients experienced lymphedema. On average, the AI tool predicted lymphedema in 81.6% of cases and correctly identified non-lymphedema cases in 72.9% of patients. Overall, the model demonstrated a predictive accuracy of 73.4%.
“Thankfully, long-term survival rates from breast cancer continue to increase, but for some patients, this means having to live with the [AEs] of their treatment. These include skin changes, scarring, lymphedema—which is a painful swelling of the arm—and even heart damage from radiation treatment,” Tim Rattay, a consultant breast surgeon and associate professor at the Leicester Cancer Research Centre of the University of Leicester, said in a press release on this project.2 “That’s why we are developing an AI tool to inform doctors and patients about the risk of chronic arm swelling after surgery and radiotherapy for breast cancer. We hope this will assist doctors and patients in choosing options for radiation treatment and reduce side effects for all patients.”
Investigators of the PRE-ACT consortium aim to devise a predictive AI tool that can provide an easily understandable explanation of AE risks in patients with breast cancer, thereby enabling shared decision-making between patients and physicians.3 Objectives of the consortium include implementing findability-accessibility-interoperability-reusability (FAIR)–compliant repositories for performing external validation of predictive models, assessing the effect of contouring variability on toxicity prediction within training cohorts, and making the model amenable to predicting AEs in other cancer types via transfer learning techniques.
“Patients identified at higher risk of arm swelling could be offered additional supportive measures, such as wearing an arm compression sleeve during treatment, which has been shown to reduce arm swelling in the long term,” Rattay added.2 “Clinicians may also use this information to discuss options for lymph node irradiation in patients, where its benefit may be fairly borderline.”
As part of the PRE-ACT initiative, investigators will use advanced machine learning methods to assess complex radiotherapy datasets, which involves combining 3D imaging with dose distribution data, genomics data, multimodal treatment data, and medical data on comorbidities as well as socioeconomic variables.4 The AI tool will include an explainability layer so that clinicians and patients alike can access explanations written in plain language. The model will also implement end-users that can supply continuous feedback to the AI system, which may help inform doctors and patients about selecting adequate radiotherapy approaches.
Investigators will further evaluate the predictive capabilities of the AI model as part of the phase 3 PRE-ACT-01 trial, which is expected to launch later in 2024. The trial will focus on collecting information related to genetic markers and imaging data to improve the AI’s predictive accuracy; such information will not be used to form predictions in the PRE-ACT trial. Investigators also plan to advance the AI tool so that it can predict other AEs such as skin and heart damage. According to Rattay, investigators anticipate an approximate enrollment of 780 patients by early 2026, and the trial will include a follow-up period of 2 years.
References
- Rattay T, Bologna G, Bombenzin-Domino A, et al. Development of an explainable AI prediction model for arm lymphoedema following breast cancer surgery and radiotherapy. Presented at the 14th European Breast Cancer Conference; March 20-22, 2024; Milan, Italy. Abstract 23.
- AI tool predicts risk of side effects after surgery and radiotherapy in breast cancer patients phase 3 clinical trial starts later this year. News release. EBCC-14 News. Accessed March 27, 2024. https://tinyurl.com/mry998mt
- Prediction of radiotherapy side effects using explainable AI. PRE-ACT. Accessed March 27, 2024. https://tinyurl.com/2ze7xd4s
- The PRE-ACT methodology. PRE-ACT. Accessed March 27, 2024. https://tinyurl.com/cwdfpvke