Alpelisib Is Changing the Clinical Landscape in Breast Cancer Treatment
The US Food and Drug Administration recently approved alpelisib plus fulvestrant for the treatment of metastatic or otherwise advanced breast cancer.
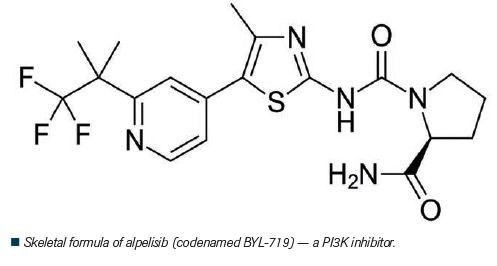
The US Food and Drug Administration (FDA) recently approved alpelisib (BYL719) plus fulvestrant for the treatment of metastatic or otherwise advanced breast cancer. Details of the drug alpelisib and its clinical approval are discussed herein.[1]
Background
Most breast cancers (>70%) are human epidermal growth factor receptor 2 (HER2)–negative and hormone-receptor (HR)–positive. Of patients living with HR-positive advanced breast cancer, approximately 40% harbor PIK3CA mutations, which hyperactivate the alpha isoform (p110α) of the phosphatidylinositol 3-kinase (PI3K) pathway.
Alpelisib is an oral α-specific PI3K inhibitor that selectively inhibits p110α to nearly 50 times stronger compared with other isoforms of the small molecule. Alpelisib has shown efficacy in targeting PIK3CA-mutated cancer based on preclinical models. When alpelisib is combined with fulvestrant, it exhibits a synergistic effect in PIK3CA-mutated, estrogen-receptor (ER)–positive xenograft models.
Specifically, alpelisib combined with fulvestrant led to a complete or partial response in 29% of patients with PIK3CA-altered, ER-positive advanced breast cancer, according to results of a phase Ib trial.[2] These effects were evident when compared with complete or partial responses in patients without PIK3CA-mutated tumors.
FDA approval
On May 24, 2019, the FDA approved alpelisib plus fulvestrant for postmenopausal women, and men, with metastatic or otherwise advanced breast cancer that is PIK3CA-altered, HR-positive, and HER2-negative.[1]
Following progression on or after endocrine-based therapy, patients amenable to treatment with alpelisib plus fulvestrant are identified via an FDA-approved diagnostic test called the therascreen® PIK3CA RGQ PCR Kit. This test uses either circulating DNA PIK3CA mutations in plasma or tissue specimens from tumors, or both, to pick out PIK3CA mutations. Specifically, if negative for PIK3CA mutations in plasma, tumor tissue is used for testing for PIK3CA mutations.
The FDA approved combined alpelisib–fulvestrant treatment based on the results of the phase III SOLAR-1 (NCT02437318) trial.[1,3]
SOLAR-1 trial
In this global, randomized, placebo-controlled trial, 572 patients (341 patients with confirmed PIK3CA mutations) were assigned to one of two cohorts based on PIK3CA-mutation status. In each group, patients were randomized to receive either 1) oral alpelisib (300 mg/d) plus fulvestrant (500 mg IM on day 1 and day15 of cycle 1 and on day 1 of subsequent 28-day cycles) or 2) placebo plus fulvestrant. Patients in each cohort were stratified per status of liver or lung metastases, as well as prior cyclin-dependent kinase 4 and 6 (CDK4/6) inhibitor treatment.[3]
At a median follow-up of 20 months in patients with PIK3CA-mutated tumors, the progression-free survival was 11.0 months (95% CI, 7.5–14.5) in the alpelisib–fulvestrant group compared with that of 5.7 months (95% CI, 3.7–7.4) in the placebo–fulvestrant group (hazard ratio, 0.65; 95% CI, 0.50–0.85; P < .001). The hazard ratio was 0.85 (95% CI, 0.58–1.25) in those without PIK3CA-mutated cancer.
Other findings included an overall response rate of 26.6% in PIK3CA-mutated cancer patients receiving alpelisib plus fulvestrant compared with that of 12.8% in those taking placebo plus fulvestrant. These values were 35.7% and 16.2%, respectively, in patients with measurable disease.
“Alpelisib has activity in patients with PIK3CA-mutated, HR-positive, HER2-negative advanced breast cancer that has progressed during or after treatment with an aromatase inhibitor,” wrote the authors. “Therefore, the integration of genomic testing for PIK3CA mutation into routine clinical practice may be useful in the selection of therapy; validated diagnostic testing procedures are not yet available.”[3]
Previous research on PI3K inhibitors has demonstrated that in patients with PIK3CA-mutated breast cancer, there was longer progression-free survival that was significant but not clinically impactful. These previous studies, however, involved the pan-PI3K inhibitor buparlisib and the β-sparing PI3K inhibitor taselisib, both of which have a narrow therapeutic index, thus resulting in off-target and discontinued treatments.
“Specific inhibition of PI3Kα may represent improved biologic targeting, a finding supported by the observed incidence of hyperglycemia of grade 3 or 4 (10.8% with taselisib vs 36.6% with alpelisib),” wrote the authors.[3]
The SOLAR-1 trial had a safety profile comparable with other trials involving alpelisib and fulvestrant. The most frequent grade 3 or 4 treatment-related adverse events were hyperglycemia (36.6% in alpelisib–fulvestrant group vs 0.7% in placebo–fulvestrant group) and rash (9.9% vs 0.3%, respectively). Furthermore, 25.0% of those taking alpelisib discontinued treatment compared with 4.2% of those taking placebo.
In total, 6.3% of patients stopped the trial secondary to hyperglycemia, which is an on-target effect of alpelisib. Hyperglycemia is yoked to α-specific PI3K inhibition; therefore, the researchers closely monitored safety to decrease participant attrition and realize maximum clinical benefit. They managed adverse events by modifying doses and providing responsive medical intervention as needed.[3]
Future directions
Standard of care for patients with HR-positive, HER2-negative advanced breast cancer is endocrine therapy plus or minus CDK4/6 inhibitors. In the future, more patients will likely receive the combination of CDK4/6 inhibitors, including ribociclib, palbociclib, and abemaciclib, and endocrine therapy for the treatment of HR-positive, HER2-negative advanced breast cancer. Nevertheless, acquired resistance to endocrine therapy is an issue. To test the efficacy of alpelisib in patients who have progressed during or after CDK4/6 inhibitor treatment, the BYLieve trial is currently enrolling patients.[4]
Certain tumors that are less sensitive to alpelisib could harbor increased concentrations of retinoblastoma protein, according to the results of preclinical studies. In these patients, a combination of PI3Kα and CDK4/6 inhibitors surmounted intrinsic and adaptive resistance in PIK3CA-mutated xenografts.[3]
Other applications
Alpelisib could be used in a wide range of solid tumors, and other indications are beginning to be explored. For example, results from a phase Ib study published in Lancet Oncology lend preliminary support to the rationale underlying the combination of poly (ADP-ribose) polymerase (PARP) inhibitors along with PI3K inhibitors in the treatment of platinum-resistant BRCA-wild type epithelial ovarian cancer. According to the authors, this combination could sensitize homologous recombination repair (HRR)-proficient epithelial ovarian cancers to PARP inhibitors, thus representing a new mechanism of action.[5]
In this trial, the 33% overall response rate of combined olaparib and alpelisib was much higher than monotherapy with either olaparib (4%–5%) or alpelisib (<5%). Of the 28 patients with epithelial ovarian cancer, 50% exhibited stable disease and 36% attained a partial response.
“Our study has shown that the combination of alpelisib and olaparib exhibits synergistic activity in BRCA wild-type, platinum-resistant ovarian cancers, thereby expanding potential use of PARP inhibitors beyond the setting of HRR deficiency, for which they currently have approval from the European Medicines Agency and US Food and Drug Administration,” wrote the authors.
They continued, “Our results and the mechanistic rationale behind PARP and PI3K inhibitor combinations might be applicable not only to BRCA wild-type, platinum-resistant ovarian cancers but also to other solid tumours with or without PI3K pathway alterations, including BRCA wild-type breast cancer, prostate, colorectal, and endometrial cancers.”[5]
Finally, results of a phase I trial indicated that 350 mg/d alpelisib monotherapy exhibited preliminary efficacy in Japanese patients with advanced solid tumors. In the study, median progression-free survival was 3.4 months, overall response rate was 3%, and disease control rate was 57.6%.[6]
FOUR KEY REFERENCES
2. Juric D, Janku F, Rodón J, et al. Alpelisib plus fulvestrant in PIK3CA-altered and PIK3CA-wild-type estrogen receptor-positive advanced breast cancer. A phase 1b clinical trial. JAMA Oncology. 2019;5:e184475.
3.. André F, Ciruelos E, Rubovszky G, et al; for the SOLAR-1 Study Group. Alpelisib for PIK3CA-mutated, hormone receptor–positive advanced breast cancer. N Engl J Med. 2019;380:1929-40.
4. ClinicalTrials.gov. Study assessing the efficacy and safety of alpelisib plus fulvestrant or letrozole, based on prior endocrine therapy, in patients with PIK3CA mutation with advanced breast cancer who have progressed on or after prior treatments (BYLieve). Available at: https://clinicaltrials.gov/ct2/show/NCT03056755. Accessed September 25, 2019.
5. Konstantinopoulos PA, Barry WT, Birrer M, et al. Olaparib and α-specific PI3K inhibitor alpelisib for patients with epithelial ovarian cancer: a dose-escalation and dose-expansion phase 1b trial. Lancet Oncol. 2019;20:570-80.
References:
1. US Food and Drug Administration. FDA approves alpelisib for metastatic breast cancer. Available at: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-alpelisib-metastatic-breast-cancer. Accessed September 25, 2019.
2. Juric D, Janku F, Rodón J, et al. Alpelisib plus fulvestrant in PIK3CA-altered and PIK3CA-wild-type estrogen receptor-positive advanced breast cancer. A phase 1b clinical trial. JAMA Oncology. 2019;5:e184475.
3. André F, Ciruelos E, Rubovszky G, et al; for the SOLAR-1 Study Group. Alpelisib for PIK3CA-mutated, hormone receptor–positive advanced breast cancer. N Engl J Med. 2019;380:1929-40.
4. ClinicalTrials.gov. Study assessing the efficacy and safety of alpelisib plus fulvestrant or letrozole, based on prior endocrine therapy, in patients with PIK3CA mutation with advanced breast cancer who have progressed on or after prior treatments (BYLieve). Available at: https://clinicaltrials.gov/ct2/show/NCT03056755. Accessed September 25, 2019.
5. Konstantinopoulos PA, Barry WT, Birrer M, et al. Olaparib and α-specific PI3K inhibitor alpelisib for patients with epithelial ovarian cancer: a dose-escalation and dose-expansion phase 1b trial. Lancet Oncol. 2019;20:570-80.
6. Ando Y, Iwasa S, Takahashi S, et al. Phase 1 study of alpelisib (BYL719), an α-specific PI3K inhibitor, in Japanese patients with advanced solid tumors. Cancer Sci. 2019;110:1021-31.