ASCO: For Painful Bone Mets, Single Fraction Irradiation Noninferior to Multiple-Fraction Therapy
The use of a single 8 Gy fraction of re-irradiation for the treatment of painful bone metastases was noninferior to multiple fractions, according to the results of the NCIC CTG SC.20 trial presented at the ASCO 2013 Annual Meeting in Chicago.
CHICAGO-The use of a single 8 Gy fraction of re-irradiation for the treatment of painful bone metastases was noninferior to multiple fractions, according to the results of the NCIC CTG SC.20 trial presented at the ASCO 2013 Annual Meeting in Chicago. However, presenter Edward Chow, MBBS, MSc, PhD, senior scientist at Sunnybrook Research Institute, pointed out that the findings were not robust, and suggested that trade-offs between pain response and acute toxicity of treatment may exist when deciding on the appropriate therapy.
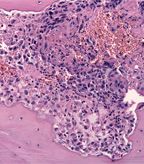
Histology of prostrate cancer infiltarting vertebral bone; source: Jensflorian, Wikimedia Commons
“Radiation is useful in palliating bone metastases, and with effective systemic treatment and better supportive care bone metastases patients actually live longer,” said Dr. Chow. “They may outlive the benefits of the initial radiation treatment; therefore, some might require repeat radiation treatment.”
Dr. Chow described three scenarios for repeat radiation therapy: no pain relief or pain progression after initial radiation therapy; partial response with initial therapy, but with the hope of further pain reduction with more radiation therapy; or partial or complete response with initial radiation therapy, but subsequent recurrence of pain.
“We know from the literature that re-irradiation works, especially in response to initial radiation,” Dr. Chow said. “There is also limited evidence that some initial nonresponders would respond to re-irradiation; however, there are currently no prospective randomized studies examining response for repeat radiation.”
Dr. Chow and colleagues conducted a study to determine if a single 8 Gy fraction of radiation was noninferior to multiple fractions for re-irradiation. The study included 850 patients aged 18 years or older with radiological confirmation of bone metastases. Patients were randomly assigned to 8 Gy radiation in one fraction or to 20 Gy in five fractions (or 8 fractions if the previous radiation was to the spine/whole pelvis).
The primary endpoint was the overall response rate at 2 months from start of treatment. The researchers used the International Consensus Endpoints, which includes pain score and analgesic consumption. Median follow-up was 12.2 months, and no difference in survival between the two treatment arms was found.
“Before the 2-month assessment, 98 patients died which constituted 11% of our patient population,” said Dr. Chow “By intention to treat, the 2-month response rate was only assessable in 62% of the patients.”
The response rate was 28% with 8 Gy compared with 32% with 20 Gy, a nonsignificant difference.
The researchers also conducted a per-protocol sensitivity analysis excluding those patients who were ineligible, inevaluable, or those who received a non-allocated therapy. The 2-month response rate was assessable in 521 patients and the response rate was 45.3% for the 8 Gy arm compared with 51.3% in the 20 Gy arm.
Seventy-seven patients in the study had pain progression, 10.6% in the 8 Gy arm and 7.5% in the 20 Gy arm, also a nonsignificant difference.
When the researchers looked at functional interference, as measured with the Brief Pain Inventory, and quality of life, as measured with the EORTC QLQ C 30, there was no significant difference between the arms over baseline or at follow-up.
Patients assigned to the multiple-fraction arm experienced significantly more skin reddening and nausea at day 7 compared to the single fraction arm. At day 14, patients in the multiple-fraction arm had higher rates of vomiting, lack of appetite, diarrhea, and skin reddening.
“Single fraction has less toxicity; single fraction is more convenient to patients, less costly to society and patients, and enhances clinical efficiency, so why hasn’t it caught on?” asked discussant Mary Uan-Sian Feng, MD, of the Comprehensive Cancer Center at the University of Michigan Health Systems.
Among the possible reasons are a fear of high doses per fraction especially to large field, a higher retreatment rate, concern about toxicity in long-term survivors and reimbursement issues, she said.