ASCO: Phase II/III Data Establish Dabrafenib as Second BRAF Inhibitor With Proven Efficacy in Metastatic Melanoma
Data from the phase III BREAK-3 and the phase II BREAK-MB trials of dabrafenib establish the drug as the second BRAF inhibitor for BRAF V600E-mutated melanoma.
CHICAGO-More mature data from the phase III BREAK-3 trial of dabrafenib vs dacarbazine (DTIC) in patients with BRAF V600E-mutated metastatic melanoma, as well as results of BREAK-MB, a phase II study assessing intracranial response to dabrafenib in patients with BRAF V600E/K-mutated melanoma and brain metastases, were presented in oral abstracts at this year's annual meeting of the American Society of Clinical Oncology (ASCO).
Taken together, these data establish dabrafenib as the second BRAF inhibitor with proven efficacy in V600-mutated melanoma, said Michael B. Atkins, MD, newly appointed deputy director of the Georgetown Lombardi Comprehensive Cancer Center, who discussed the two abstracts. “FDA approval should happen,” he said.
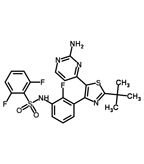
Chemical structure of dabrafenib
Axel Hauschild, MD, of the University of Kiel in Germany, presented the updated data from the BREAK-3 trial. He noted that although the BREAK-3 data that were presented at ASCO 2011 were promising, they were still immature. Now, a year later, the data continue to show significantly improved efficacy of dabrafenib compared with DTIC. Treatment-nave patients with unresectable stage III or IV BRAF V600E-mutated melanoma were randomized in a 3:1 design to dabrafenib, 150 mg bid or DTIC, 1000 mg/m2 q3w. The primary endpoint of the study was progression-free survival; secondary endpoints included overall survival, response rate, duration of response, and safety. Fifty percent of the patients who received dabrafenib were classed as responders, including 3% with complete responses. Median progression-free survival was 5.1 months in the dabrafenib cohort vs 2.7 months in the DTIC group; the decline in the risk of progression or death with dabrafenib was 70% compared with DTIC. Although it is still too early to have overall survival data, Dr. Atkins predicted that these would likely be similar to those seen with vemurafenib.
However, Dr. Atkins pointed out that there were some significant differences between the toxicity profile of dabrafenib and that of vemurafenib. Treatment-related adverse events seen with dabrafenib in BREAK-3 were mainly dermatologic: skin lesions such as squamous cell carcinomas occurred in 7% of patients. By contrast, these sorts of dermatologic adverse events are typically seen in 11% of patients treated with vemurafenib. Phototoxicity also occurred far less frequently in patients treated with dabrafenib than is seen with vemurafenib treatment (3% vs 41%). Of note, however, new primary melanomas were seen in three patients treated with dabrafenib in the BREAK-3 trial, and pyrexia occurred in 15% of the dabrafenib-treated cohort.
John M. Kirkwood, MD, of the University of Pittsburgh Cancer Institute, presented data from BREAK-MB. Dr. Kirkwood pointed out that brain metastases are common in advanced melanoma: they are seen in 20% to 25% of patients with stage IV disease. And until the advent of the BRAF inhibitors, there were no systemic therapies with activity against these lesions.
There were preclinical data and murine data demonstrating the ability of dabrafenib to penetrate the brain, and phase I data showed that dabrafenib had clinical efficacy in BRAF V600E-mutated patients with previously untreated brain metastases (8 out of 10 patients had objective responses, 4 of whom had complete responses). These results provided the impetus for a phase II study.
The phase II trial involved 172 patients, 41 of whom had reached 8-week disease assessment and thus could be included in this interim analysis. Some patients had received prior brain therapy, and others had experienced progression following prior brain therapy. Overall (unconfirmed) intracranial response rate was 53% in the patients with V600E mutations. The overall response rate (complete responses plus partial responses) in these patients was between 40% and 53% (depending on prior therapy). Somewhat lesser responses were seen in the patients with V600K mutations. Between 19% and 24% of patients experienced grade 3/4 toxicities, a rate the investigators deemed acceptable.
Dr. Kirkwood concluded: “This unprecedented response rate and survival shifts the paradigm we’ve seen in the past not to enroll patients with brain disease in systemic therapies.” And Dr. Atkins, in his discussion of the BREAK-MB results, noted that dabrafenib now made it possible to view brain metastases as “just another metastatic site.” In fact, he suggested that the intracranial efficacy demonstrated by dabrafenib might be sufficient to consider it as a replacement for whole-brain radiation therapy.