ASCO: Ponatinib Provides New Option for Heavily Treated Patients With CML
Updated clinical data from the pivotal phase II global PACE trial of ponatinib confirm its impressive antileukemic activity in patients with chronic myeloid leukemia or Philadelphia-chromosome-positive acute lymphoblastic leukemia at all stages who are resistant or intolerant to dasatinib or nilotinib.
CHICAGO-Updated clinical data from the pivotal phase II global PACE trial of ponatinib “confirm its impressive antileukemic activity in patients with chronic myeloid leukemia (CML) or Philadelphia chromosome–positive acute lymphoblastic leukemia (Ph+ ALL) at all stages who are resistant or intolerant to dasatinib or nilotinib, or who have the T315I mutation for which there are no currently available treatments,” reported Jorge Cortes, MD, professor and deputy chair, department of leukemia at the University of Texas MD Anderson Cancer Center in Houston. He presented efficacy and safety data on 444 treated patients in six prespecified cohorts at 45 mg of ponatinib administered orally once daily.[1]
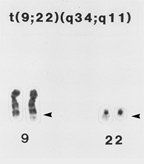
Philadelphia chromosome: partial karyotype of a myeloid cell from the bone marrow of a patient with CML showing the typical t(9;22) translocation.
These data show that 54% of chronic-phase CML patients in the trial, including 70% percent of patients who have a T315I mutation, achieved a major cytogenetic response. “Clinical responses to ponatinib were observed in patients regardless of their mutation status or disease stage,” said Cortes. “Of particular importance, responses to ponatinib appear to be durable, with 93% of chronic-phase CML patients projected to remain in major cytogenetic response at one year.”
Patients were assigned to a cohort based on their phase of disease (chronic-phase, accelerated-phase or blast-phase CML/Ph+ ALL) and T315I mutation status (with or without the mutation).
Ninety-three percent of the patients in the trial had received at least two tyrosine kinase inhibitors (TKIs) prior to enrollment; 58% had received three or more TKIs prior to enrollment. Chronic-phase patients had bone marrow assessments approximately every 3 months to determine cytogenetic response. Findings were based on at least 6 months of available response data.
Based on assessment of 267 evaluable chronic-phase CML patients in the trial, 54% (144 patients) achieved a major cytogenetic response, with 44% achieving a complete cytogenetic response. Median follow-up of the chronic-phase CML patients is 10.1 months. Major cytogenetic response is the primary endpoint for chronic-phase CML patients in the ongoing trial.
Of 64 evaluable chronic-phase CML patients with the T315I mutation, 70% (45 patients) achieved a major cytogenetic response, with 66% achieving a complete cytogenetic response. The major cytogenetic response rate in 203 evaluable chronic-phase patients without the T315I mutation was 49% (99 patients).
Of 267 chronic-phase patients, 30% (79 patients) achieved a major molecular response. Of 64 chronic-phase patients with the T315I mutation, 50% (32 of 64) attained a major molecular response. (Major molecular response is the primary endpoint in a planned phase III trial expected to begin later this year.)
Twenty-one chronic-phase patients treated with ponatinib in the PACE trial had previously received treatment with only one TKI. Thirteen had been treated with imatinib only and eight had received either dasatinib or nilotinib. Of the 21 patients who had received treatment with only one TKI prior to receiving ponatinib, 86% (18 patients) achieved a major cytogenetic response.
Sixty percent (39 of 65) of accelerated-phase patients in the resistant or intolerant cohort achieved a major hematologic response. Fifty percent (9 of 18) of accelerated-phase patients with the T315I mutation achieved a major hematologic response, the primary endpoint in accelerated and blast-phase CML or Ph+ ALL patients in the trial.
Thirty-five percent (17 of 48) of blast-phase CML or Ph+ ALL patients in the resistant or intolerant group achieved a major hematologic response. Similarly, 33% percent (15 of 46) of blast-phase CML or Ph+ ALL patients with the T315I mutation also had a major hematologic response. Thirty-four percent (22 of 65) of accelerated phase patients and 27% (13 of 48) of blast phase or Ph+ ALL patients in the resistant or intolerant cohorts achieved a major cytogenetic response; 20% (13 of 65) of patients in accelerated phase and 23% (11 of 48) of patients in blast phase or Ph+ ALL in this same group achieved a complete cytogenetic response.
Updated safety data on 444 patients suggest that ponatinib has a favorable profile in these heavily pretreated patients. The most common adverse events considered related to ponatinib included thrombocytopenia in 35% of patients, rash (32%), dry skin (30%), abdominal pain (22%), and headache (18%). Elevated serum lipase, fatigue and arthralgia were observed less frequently. The incidence of pancreatitis across the study and including all grades was 6%. Pancreatitis was previously determined to be the dose-limiting toxicity of ponatinib in the phase I trial.
“In this multicenter, phase II trial, ponatinib was found to be safe and effective in patients in which at least two TKIs have failed or who have the T315I mutation,” commented Olatoyosi Odenike, MD, associate professor of medicine at the University of Chicago, who specializes in treatment of adults with leukemia, chronic myeloproliferative diseases, and myelodysplastic syndromes. “There are three TKIs currently approved for front-line treatment in CML, but there is currently no treatment option available for individuals with the T315I mutation. This provides a new treatment option for the heavily pretreated patients with CML, including patients with the T315I mutation.”
Ponatinib is being developed by ARIAD Pharmaceuticals, Cambridge, Mass.
Reference
1. Cortes JE, Kim DW, Pinilla-Ibarz J, et al. PACE: A pivotal phase II trial of ponatinib in patients with CML and Ph+ALL resistant or intolerant to dasatinib or nilotinib, or with the T315I mutation. J Clin Oncol. 2012;30:(suppl; abstr 6503).