ASCO Recommends All Breast Cancer Patients Receive HER2 Testing
New ASCO and CAP guidelines recommend HER2 testing for all newly diagnosed breast cancer patients with either early-stage invasive or metastatic disease.
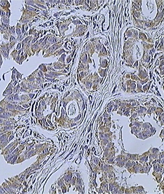
Infiltrating ductal carcinoma of the breast assayed with anti-HER2 antibody. Source: Itayba, Wikimedia Commons.
Guidelines on HER2 testing in patients with invasive breast cancer by the American Society of Clinical Oncology (ASCO) and the College of American Pathologists (CAP) have been updated for the first time since their publication in 2007.
The guidelines recommend HER2 testing for all newly diagnosed breast cancer patients with either early-stage invasive or metastatic disease. The new update is based on a new review of the literature.
The guide is a tool for pathologists and oncologists that shows how to test and interpret the results of HER2 overexpression assays, and recommends therapies for HER2-positive breast cancer. The guidelines are published in the Journal of Clinical Oncology and the Archives of Pathology and Laboratory Medicine.
“One of the key features of the guideline update is our ability to better discriminate between HER2-positive and negative results, thereby reducing the frequency of equivocal or inconclusive test results,” said Antonio Wolff, MD, co-chair of the guidelines steering committee and professor of oncology at Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University in Baltimore, Maryland. “This together with better standardization tissue handling, laboratory performance of HER2 testing, and reporting of test results in the US and elsewhere allowed us to be more specific about less common clinical scenarios, with the ultimate goal of giving clinicians and patients the best possible information to allow individualized clinical decision-making.”
The approximate 15% of patients with newly diagnosed breast cancer whose tumors are HER2-positive have a higher level of expression of the HER2 protein on their tumor. Several therapies for HER2-positive breast cancer are now approved by the US Food and Drug Administration (FDA), including the antibodies trastuzumab (Herceptin), pertuzumab (Perjeta), and trastuzumab emtansine (T-DM1; Kadcyla), and the oral agent lapatinib (Tykerb). HER2-specific therapies have substantially improved the outcomes for women with HER2-positive cancer, which is a relatively aggressive form of breast cancer.
Two FDA-approved testing methods-immunohistochemistry (IHC) or in situ hybridization (ISH)-are used on a tumor sample to assay for amplification of the HER2 gene. If the test result is equivocal, the guidelines recommend re-testing, using the alternative test on the same tumor specimen or another tumor sample.
In rare cases where testing of tumor samples results in an equivocal result, the guidelines suggest clinicians should consider all available clinical data on the patient before recommending HER2-targeted therapy. HER2-targeted agents should not be given to a patient whose tumor is HER2-negative.
IHC assesses the level of the HER2 protein on the surface of tumor cells, while ISH detects the number of copies of HER2 that are in the genomes of tumor cells. The previous guidelines recommended only fluorescence in situ hybridization (FISH) to evaluate for HER2 gene amplification, but the new guidelines also includes bright-field ISH, which uses a regular light microscope rather than a fluorescent microscope. FISH was the standard ISH reference assay used in the early trials that demonstrated benefit from HER2-targeted therapies but is expensive, requires specialized equipment, and can be technically challenging. Bright-field ISH is an alternative method that does not require a specialized fluorescent microscope, allows side-by-side evaluation with the routine histology slide and-if needed-with a HER2 IHC slide, and provides similar information when properly done.
“The number of patients with equivocal HER2 test results used to be rather large. But evidence suggests that the quality of HER2 testing is improving, and the frequency of equivocal and inaccurate results is decreasing,” said Elizabeth H. Hammond, MD, co-chair of the guidelines steering committee and professor of pathology at the University of Utah School of Medicine, in a statement. “We believe that this is at least in part due to our earlier recommendations in 2007. We hope the current guideline will resolve remaining challenges in the field, and ultimately result in better outcomes for all patients with breast cancer.”
The guidelines also emphasize the need for collaboration among physicians, laboratories, and other health care providers for the treatment of women with breast cancer, and in performing and interpreting molecular tests that greatly influence treatment.