ASH: Quizartinib Active in Subset of AML Patients
Final results of a cohort from a phase II monotherapy trial of quizartinib in acute myeloid leukemia patients showed that more than half of patients 60 years of age and older who harbored an internal tandem duplication in the FMS-like tyrosine kinase 3 had a composite complete remission.
Final results of a cohort from a phase II monotherapy trial of quizartinib in acute myeloid leukemia (AML) patients showed that more than half of patients 60 years of age and older who harbored an internal tandem duplication in the FMS-like tyrosine kinase 3 (FLT3-ITD) had a composite complete remission. Patients who were negative for the FLT3-ITD mutation also responded, but to a lesser extent. Of those patients who were refractory to their last AML treatment, 41% responded to quizartinib. The data was presented by Jorge Cortes, MD, of the department of leukemia at the MD Anderson Cancer Center in Houston, Texas, at the annual American Society of Hematology (ASH) meeting held in Atlanta.
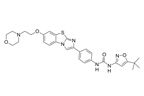
Chemical structure of quizartinib
Eight percent of patients in this study were able to transition from quizartinib to a hematopoietic stem cell transplantation (HSCT), which has a chance to be curative.
The first cohort of the study included 134 patients 60 years old or older who had relapsed after first-line chemotherapy within 1 year of treatment. Of these patients, 69% (92 patients) were positive for FLT3-ITD, 31% (41 patients) were FLT3-ITD negative and 1% had an unknown FLT3-ITD status.
Patients took quizartinib once daily starting at 90 mg or 135 mg for 28-day cycles.
Quizartinib, developed by Ambit Biosciences together with Astellas Pharma Inc, is an oral selective inhibitor of FLT3 and KIT, both tyrosine kinases. Quizartinib has been shown to be active against both mutated and wild type versions of the FLT kinase, although higher activity is detected among FLT3-mutated patients.
The FLT3 gene is among the most frequently mutated in AML patients. Approximately 30% of AML patients harbor this type of genetic mutation. The FLT3-ITD mutation makes a protein that is always active, signaling to bone marrow stem cells to constantly grow and divide. This mutation results in a more aggressive, faster growing form of AML which is associated with more frequent relapse after chemotherapy treatment. Change in mutation status often occurs during treatment-both change to a mutation in FLT3 and reversion to wild type have been documented. Besides internal tandem repeats of the gene, point mutations also occur; thus far, no difference in survival have been found among patients with either type of FLT3 mutation.
More patients with an FLT3-ITD mutation responded to quizartinib compared to those who were FLT3-ITD negative in the study: 54% (50 patients) of those who were FLT3-ITD positive had a composite complete remission compared to 13% (32 patients) who were FLT3-ITD negative. Composite complete remission was defined as the combination complete remissions, complete remissions with incomplete platelet recovery, and complete remissions with incomplete hematologic recovery. 51% of the FLT3-ITD–positive patients had complete remissions with incomplete hematologic recovery. Median duration of response for these patients was 12.7 weeks and had a median overall survival time of 25.3 weeks. The median duration of response for FLT3-ITD–negative patients was 22.1 weeks and a median overall survival of 19.0 weeks. Both patient types of patients who were also refractory to their last AML treatment responded to quizartinib: 39% and 44% of FLT3-ITD–positive and FLT3-ITD–negative patients, respectively.
Treatment discontinuation due to a treatment-related event occurred in 13% of the 134 patients. Common adverse events that were treatment-related included nausea (40%), fatigue (31%), anemia (28%), QT interval prolongation (25%), diarrhea (23%), vomiting (23%), dysgeusia (22%), and febrile neutropenia (20%). High-grade adverse events occurring in more than 10% of patients included anemia (25%), febrile neutropenia (20%), and thrombocytopenia (12%). High grade QT interval prolongation occurred in 13% of patients including one grade 4 event.
In a separate presentation on the second cohort in this 333-patient phase II study, 137 patients 18 years or older with relapsed or refractory AML were given quizartinib as a second-line therapy after either chemotherapy or HSCT. Similar to the results with older patients, FLT3-ITD–positive patients were more likely to respond to quizartinib. About one-third of this younger patient cohort successfully bridged to HSCT. Mark J. Levis, MD, PhD of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University in Baltimore showed that 44% (44 of 99) of FLT3-ITD–positive patients and 34% (13 of 38) FLT3-ITD patients achieved a composite complete remission. The majority of the responses in both subgroups were complete remissions with incomplete hematologic recovery.
The adverse event profile was similar to that of the older patient cohort but no grade 4 QT interval prolongation occurred. Discontinuation due to treatment-related toxicities occurred in 10% (14) of patients.
According to the study researchers, “these data represent the highest level of single agent activity observed to date for FLT3-targeted therapy in elderly patients with relapsed/refractory FLT3-ITD–positive AML.”
Final results of another phase II trial testing quizartinib post-stem cell transplant or after second-line chemotherapy will be presented at the ASH meeting on Monday, December 10, 2012. Ambit Biosciences is currently planning larger phase III trials comparing quizartinib to chemotherapy in patients with the FLT3 mutation based on these trial results.