Assessing Differences in Cancer Incidence and Mortality in Hispanic/Latinx Vs Non-Hispanic White Populations
CancerNetwork® sat down with Ruben Mesa, MD, to discuss the disparities present in Hispanic and Latinx patients with cancer.
During Hispanic Heritage Month, CancerNetwork® spoke with Ruben Mesa, MD, executive director of Mays Cancer Center, home to The University of Texas San Antonio MD Anderson, about disparities in incidence and outcomes in Hispanic and Latinx patients with cancer. Importantly, Mesa drills down into how every step of care from preventative care to screenings to treatment play a role in these disparities.
“Catching cancer in its earliest stages is critical. Both screening as well as access to care [in the face of] symptoms is critical. Next, access to a prompt evaluation and the full spectrum of services for cancer [should be considered]. Sometimes [disparities] can be related to everything, such as adequate testing of the cancer because of insurance or lack of insurance won't cover state of the art genetic testing technology that helps to determine how [the disease] should be treated. Or it can impact the access to some of the expensive cancer therapies or drugs, or the other supportive care options. Finally, it can have an impact on really dealing with complications and survivorship care,” Mesa said. “The outcomes can be worse clearly in Latinos with cancer as it can be with other underrepresented groups, in particular, for this full spectrum of reasons.”
A report from the American Cancer Society estimated that 80,200 new cases of cancer would be diagnosed in Hispanic men plus 96,400 in Hispanic women.1 While the number 1 cause of death in non-Hispanic White individuals is heart disease, the leading cause of death in Hispanic individuals is cancer, with an experts estimating that 23,800 men and 22,700 women will die from cancer in 2021. Notably, lung cancer was reported to be the leading cause of death in Hispanic men and breast cancer in women.
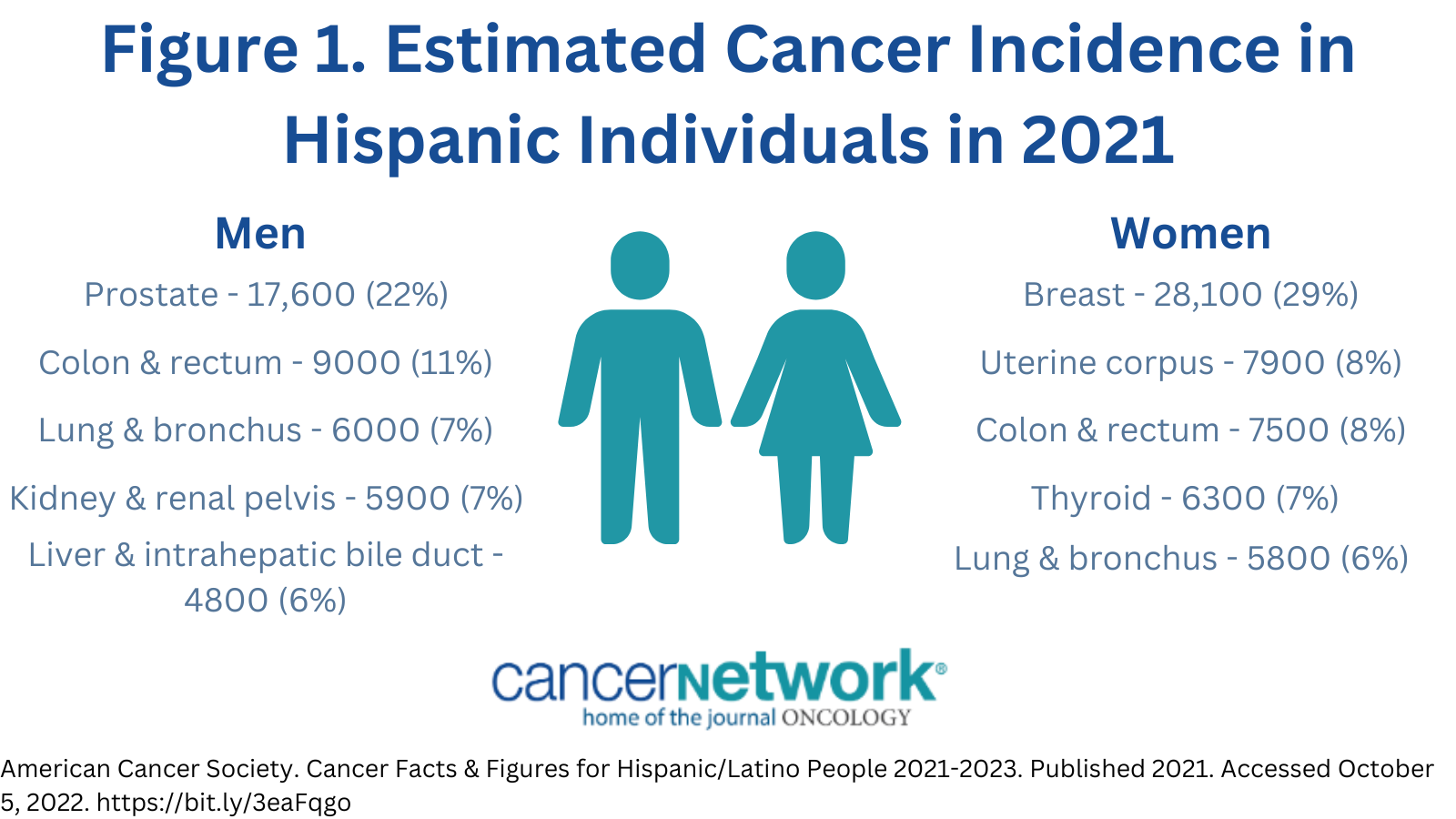
The report noted that from 2009 to 2018, cancer incidence in men decreased by approximately 2% and was stable in women. Although cancer incidence was still 5% higher in men than it was in women in 2018, that gap appears to be closing. Moreover, cancer mortality decreased from 2010 to 2019 in Hispanic men by 1.6% and 0.9% in Hispanic women compared with 1.8% and 1.5% in respective non-Hispanic counterparts.(FIGURE1)
FIGURE1. Estimated Cancer Incidence in Hispanic Individuals in 2021
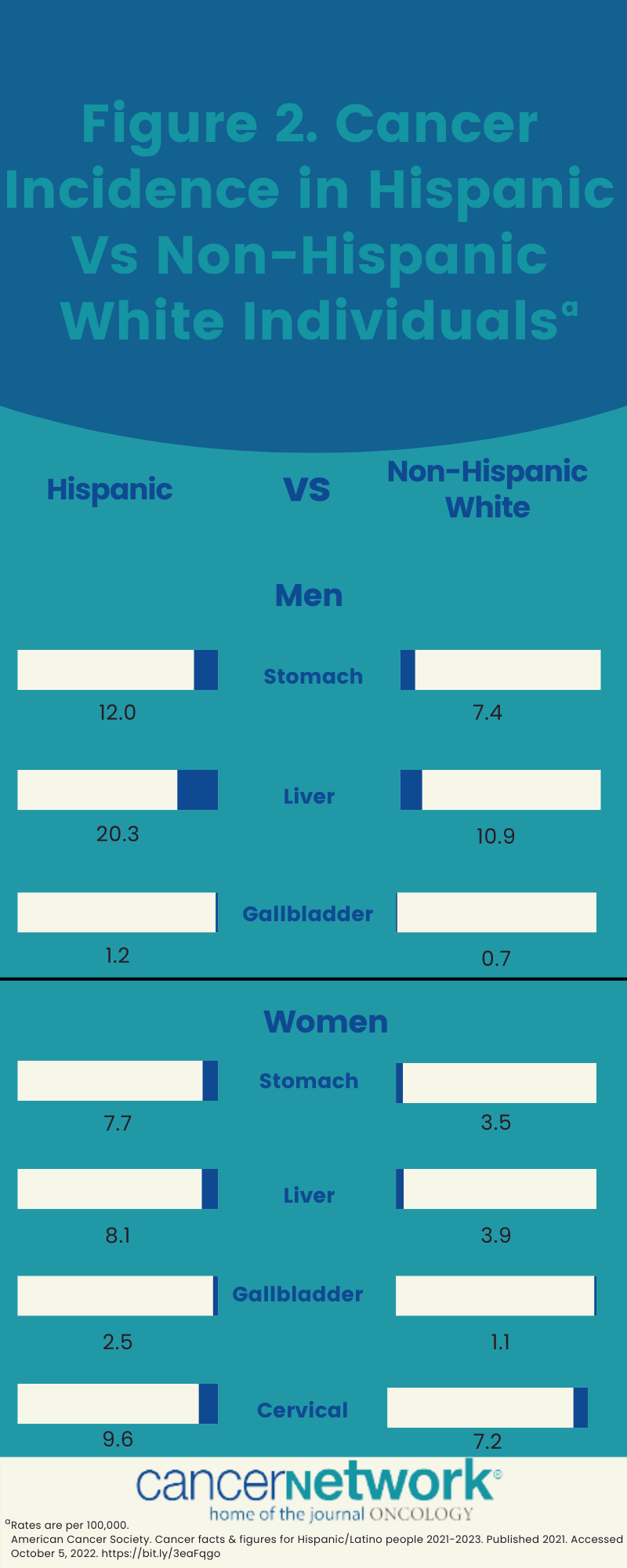
Notably, the Hispanic population in the United States were less likely to develop breast, colorectal, lung, and prostate cancer compared with non-Hispanic White individuals, but were more likely to develop cancers related to infection, such as stomach, liver, cervical, and gallbladder cancer. Although this is reflective of cancer incidence in Latin America, significant variation was observed regarding country or origin and nativity, with risk level in long-term residents and descendants approaching or overtaking what has been observed in non-Hispanic White individuals in certain diseases.
“Disparities and challenges with equity in cancer are a major issue,” Mesa said. “In cancer, it crystallizes in many ways to decrease the burden of cancer in San Antonio, South Texas. [It’s] a region of 38 counties of South Texas that is [composed of 69% Latinx individuals]. The health disparities really begin on the front end in terms of cancer prevention.”
Although 5-year relative survival was comparable between Hispanic and non-Hispanic White individuals, the 5-year survival rates for men diagnosed with melanoma were 78% vs 91%, respectively; corresponding rates were 88% vs 95% in women.1 This is likely reflective of a later stage of disease at diagnosis or even a higher likelihood of thicker tumors within the Hispanic population. In particular, children and adolescents of Hispanic and Latinx heritage have a higher cancer incidence and worse 5-year OS compared with White patients in the same age groups.(FIGURE2)2
FIGURE2. Cancer Incidence in Hispanic Vs Non-Hispanic White Individuals
“Importantly, broader survival disparities among Hispanic individuals may be masked because follow-up is more challenging and less accurate for people who are foreign-born and may return to their home country with illness,” according to the report. “Survival comparisons are also influenced by the younger age structure among Hispanic individuals because unlike incidence and mortality, survival statistics as reported by the National Cancer Institute’s Surveillance, Epidemiology, and End Results program are not adjusted for age.”
Be sure tp read part 2 of our Hispanic Heritage Month series examining clinical trial disparities for Hispanic/Latinx patients.
References
- American Cancer Society. Cancer Facts & Figures for Hispanic/Latino People 2021-2023. Published 2021. Accesssed October 5, 2022. https://bit.ly/3eaFqgo
- Aristizabal P, Winestone LE, Umaretiya P, et al. Disparities in pediatric oncology: the 21st century opportunity to improve outcomes for children and adolescents with cancer. Am Soc Clin Oncol Edu. 2021;41: e315-e326. doi:10.1200/EDBK_320499