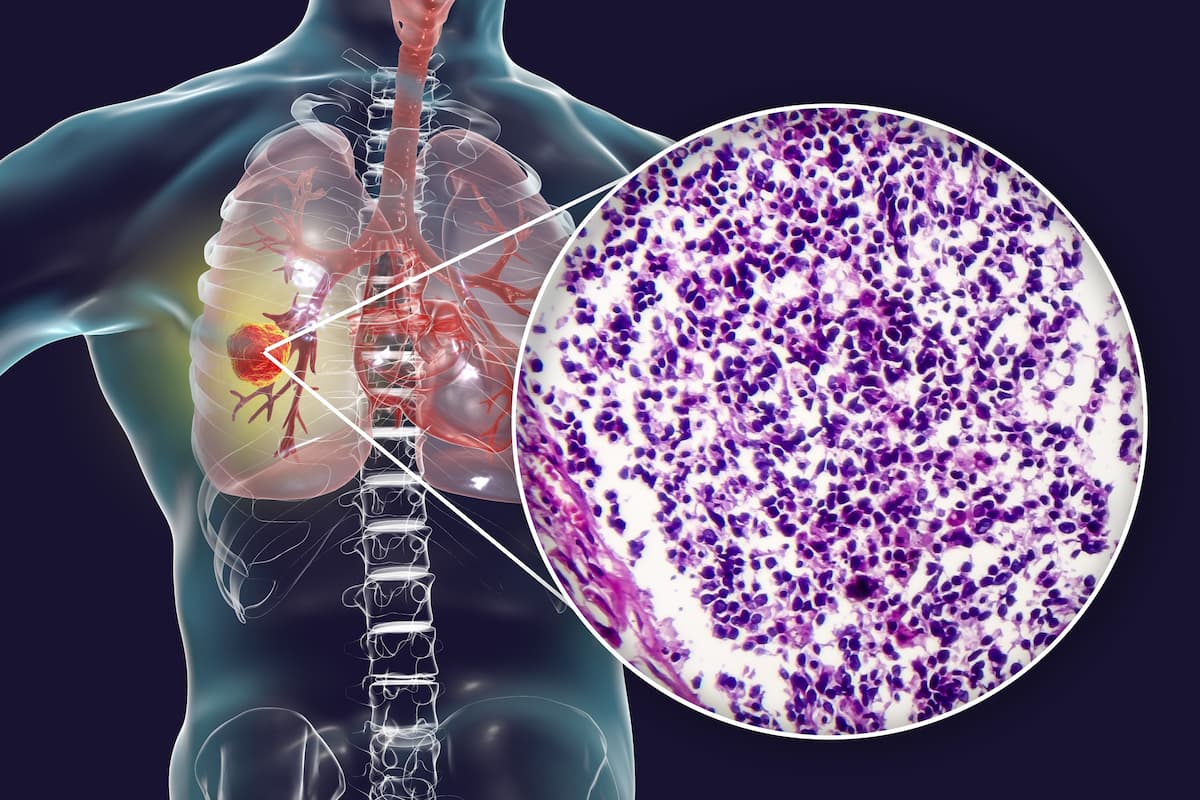
ASTRO/ESTRO Guideline Touch on Local Therapy in Oligometastatic NSCLC
An update to the ASTRO and ESTRO clinical guidelines highlights the importance of a multidisciplinary approach to treating oligometastatic non–small cell lung cancer.
The American Society for Radiation Oncology (ASTRO) and the European Society for Radiotherapy and Oncology (ESTRO) released an updated clinical guideline on how to best use definitive local therapy in patients with oligometastatic non–small cell lung cancer (NSCLC).1
"Oligometastatic NSCLC is a phase in lung cancer development that may offer us new opportunities to improve patient outcomes because it typically is more treatable than widely metastatic cancer," according to an expert from The University of Texas, Southwestern Medical Center in Dallas.
The authors indicated that the clinical benefit of local therapy on patient outcomes isn’t largely available for patients with oligometastatic disease. As data are quickly evolving and are reading out in support of the use of oligometastatic NSCLC, the guidelines set out to highlight the recommendations as a function of the data quality to better guide decisions using a multidisciplinary, patient-centered approach.
The approach was strongly recommended for all decision-making due to a significant lack of randomized phase 3 trials. The authors emphasized that local therapy should only be used if it is determined to be feasible and safe for all disease sites; this was clarified to be 5 or fewer distinct sites. In particular, the guideline highlighted conditional recommendations for definitive local therapies in the cases of extracranial disease that is synchronous, metachronous, oligopersistent, and oligoprogressive conditions.
“Oligometastatic NSCLC is a phase in lung cancer development that may offer us new opportunities to improve patient outcomes because it typically is more treatable than widely metastatic cancer,” Puneeth Iyengar, MD, PhD, co-chair of the guideline task force and an associate professor of radiation oncology at the University of Texas, Southwestern Medical Center in Dallas, said in a press release.2
“The research on local therapy for oligometastatic cancer is still at a relatively early stage, but we already see indicators of potential benefits for patients. Adding local therapy to systemic therapy may lead to more durable cancer control, potentially improving progression-free survival, overall survival, and quality of life.”
The only primary definitive local therapy modalities that were recommended for the treatment of oligometastatic disease were radiation and surgery. The guideline also detailed sequencing recommendations for systemic and local therapy integration, as well as recommendations for the best use of local hypofractionated or stereotactic body radiotherapy.
The guideline task force included a multidisciplinary team of radiation, medical, and surgical oncologists across the United States and Europe, including a radiation oncology resident, a pulmonologist, thoracic surgeons, a medical physicist, and a patient representative. The task force conducted a systemic search of human participant studies via the Ovid MEDLINE database, for English publications with dates ranging from January 2006 to February 2022.
The authors included randomized clinical trials, meta-analyses, and prospective and retrospective trials; retrospective trials with less than 50 patients were excluded from the search. Patients in the trials also needed to be 18 years of age or older with oligometastatic NSCLC.
“Despite the widespread enthusiasm in the field of oligometastatic disease, the quality of evidence supporting the integration of definitive local therapy into a multimodality treatment strategy is still lower as compared [with] indications such as locally advanced NSCLC,” Matthias Guckenberger, MD, co-chair of the guideline task force and a professor and chairman of radiation oncology at the University Hospital Zurich in Switzerland, explained.
“To compensate for this lack of highest-quality evidence, recommendations of this guideline were established by a broad consensus involving experts from ASTRO and ESTRO, colleagues from the fields of thoracic surgery and medical oncology, and a patient representative.”
The guideline states that patients with NSCLC may present with multiple—sometimes indolent—synchronous primary cancers, true oligometastatic disease needs to be confirmed in patients presenting with multiple lung lesions at initial diagnosis or following a disease-free interval.
If imaging and pathologic workup are not enough to differentiate between oligometastatic disease and multiple synchronous or repeated primary NSCLC, patients should be considered and treated as having multiple synchronous primaries. Additionally, if patients with oligometastatic disease have a good performance status, they should be considered eligible for local therapy; patients with an ECOG performance status of 2 should also be considered for definitive local therapy following systemic therapy.
Appropriate imaging is of notable importance in patients with oligometastatic disease due to a current lack of biomarkers. Several organizations including the European Society of Medical Oncology, the National Comprehensive Cancer Network, and the European Organisation for Research and Treatment of Cancer recommend contrast-enhanced chest and upper abdomen CT scan at minimum with a preference for whole body 18-FDG-PET-CT scan.
MRI brain scans are also recommended. A biopsy can be used to confirm metastatic disease in a least 1 lesion.
The guideline also recommends the use of locoregional therapy for residual primary tumors and mediastinal nodes following induction systemic therapy. Moreover, holistic consideration for patients and their disease is now the standard, although historically, distinctions were made between brain and extra-cranial metastases; this includes cranial and extra-cranial disease in the oligometastatic state. Neither radical nor safe targeting should be used even when considering the number of lesions, size, and location.
References
- Iyengar P, All S, Berry MF, et al. Treatment of oligometastatic non-small cell lung cancer: an ASTRO/ESTRO clinical practice guideline. Pro Prac Rad Onc. Published online April 25, 2023. doi:10.1016/j.prro.2023.04.004
- ASTRO and ESTRO issue clinical guideline on local therapy for oligometastatic lung cancer. News release. American Society for Radiation Oncology (ASTRO). April 25, 2023. https://bit.ly/427Mf61