Atezolizumab/Vaccine Combo May Show Long-Term Survival in ES-SCLC
Data show that XCR1-positive conventional type 1 dendritic cells may play a role as mediators of response to atezolizumab in extensive-stage SCLC.
"DC vaccination plus atezolizumab demonstrated a favorable safety profile with long-term survivors," according to the study authors.
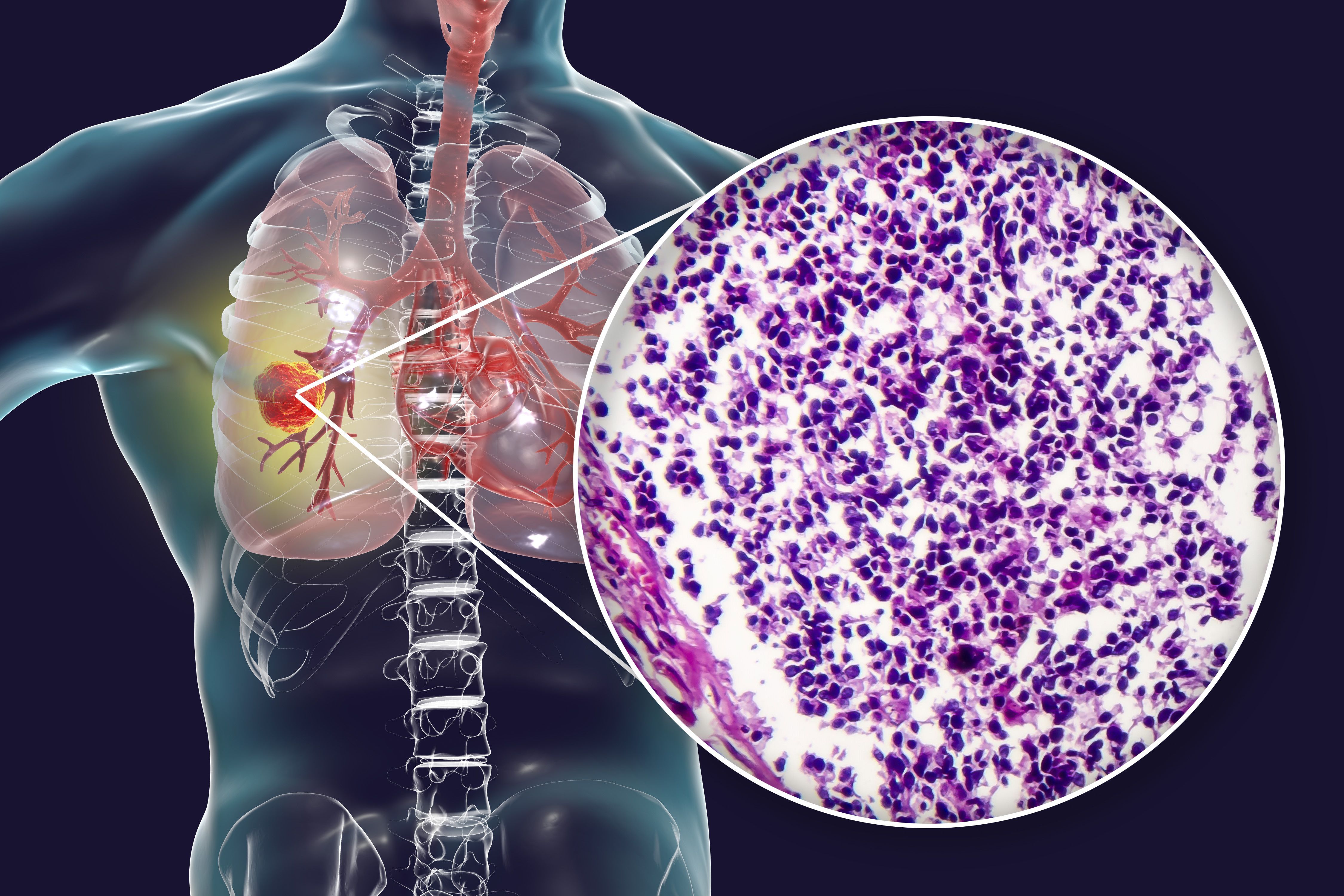
Combining dendritic cell (DC) vaccination with atezolizumab (Tecentriq) produced long-term survival in a small cohort of patients with extensive-stage small cell lung cancer (ES-SCLC), according to findings from a phase 1b/2 trial (NCT04487756) presented in a poster session at the Society for Immunotherapy of Cancer 2025 Annual Meeting in National Harbor, Maryland.1
After a median follow-up of 25.7 months among 18 patients who received DC vaccination at a median of 3 doses (range, 1-6), data showed a median progression-free survival (PFS) of 4.7 months (95% CI, 4.2-6.9) and a median overall survival (OS) of 11.2 months (95% CI, 6.3-17.9). Survival beyond 24 months occurred in 33% (n = 6) of patients; 22% (n = 4) achieved progression-free status at this time. Investigators reported no significant differences in long-term survival outcomes based on clinical features, PD-L1 expression, molecular subtype of SCLC, or tumor mutational burden (TMB).
Investigators observed an expansion of XCR1-positive conventional type 1 DCs (cDC1s; P = .03) and CXCR5-positive, PD-1–positive, CD8-positive T cells (P = .05) following induction in patients with long-term survival. The median OS was 6.7 months (95% CI, 5.0-11.6) in patients with CXCR5-positive, PD-1–positive T-cell changes of less than 0.42 vs 26.0 months (95% CI, 6.8-not accessible [NA]) in those with a change of 0.42 or higher. Regarding the expansion of XCR1-positive DCs within cDC1, the median OS was 6.3 months (95% CI, 5.0-11.6) in those with a change of less than 0 vs 19.0 months (95% CI, 6.8-NA) in those with a change of 0 or more.
The median OS was 16.2 months (95% CI, 7.0-NA) in patients with a DC1 percentage expansion of 0.77 or lower following DC vaccination and 6.5 months (95% CI, 6.3-6.8) in those with a change of more than 0.77. Regarding percentage expansion of type 2 DC following vaccination, the median OS was 26.0 months (95% CI, 6.3-NA) in patients with a change of 9 or lower compared with 8.9 months (95% CI, 6.3-11.6) in those with a change of more than 9.
“DC vaccination plus atezolizumab demonstrated a favorable safety profile with long-term survivors,” Maria González-Cao, MD, from Dexeus University Hospital in Barcelona, Spain, wrote with coauthors in the poster.1 “Results suggest a role of [XCR1-positive] cDC1s as mediators of response to atezolizumab.”
Investigators of the multicenter, open-label study assessed DC vaccination as a therapeutic agent and as a potential mediator of immune response elicited with atezolizumab among 20 patients with ES-SCLC. Patients received standard induction with chemotherapy plus atezolizumab followed by a maximum of 6 doses of 10 x 106 mature DCs via intradermal administration and atezolizumab at 1200 mg intravenously every 3 weeks. Investigators assessed DC populations and exhausted CD8-positive T-cell subsets in patient blood samples using flow cytometry, defining long survival at an 18-month cutoff.
The trial’s primary end points included PFS at 6 months and the frequency and severity of adverse effects (AEs) and serious AEs.2 Secondary end points included duration of clinical benefit, OS, and objective response rate.
Patients 18 years or older with histologically confirmed ES-SCLC and centrally confirmed tumor tissue viability for vaccine preparation were eligible for enrollment in the trial. Other eligibility criteria included having no prior cancer treatment in the advanced setting, a minimum life expectancy of 16 weeks, and an ECOG performance status of 0 or 1.
Investigators categorized 6 patients as long survivors and 12 others who were not long survivors. The median age was 60 years (range, 53-75) and 62 years (range, 54-73), respectively, and most patients in each respective group were women (50% vs 58%). More patients with long survival had brain metastases (50% vs 17%), whereas a higher proportion of those without long survival had bone metastases (0% vs 50%). Among 3 and 9 evaluable patients in each group, the median TMB was 29 (range, 24-30) and 23 (range, 20-29), respectively.
References
- Gonzalez-Cao M, Sistere-Oro M, Moran T, et al. Long term survivors from phase Ib-II trial of tumor-loaded monocyte-derived dendritic cell vaccination plus atezolizumab in ES-SCLC. Abstract presented at: Society for Immunotherapy of Cancer 2025 Annual Meeting; November 5-9, 2025; National Harbor, MD. Abstract 350.
- Combination of atezolizumab with dendritic cell vaccine in patients with lung cancer (VENEZO-LUNG). ClinicalTrials.gov. Updated April 3, 2024. Accessed November 13, 2025. https://tinyurl.com/598uuhw9