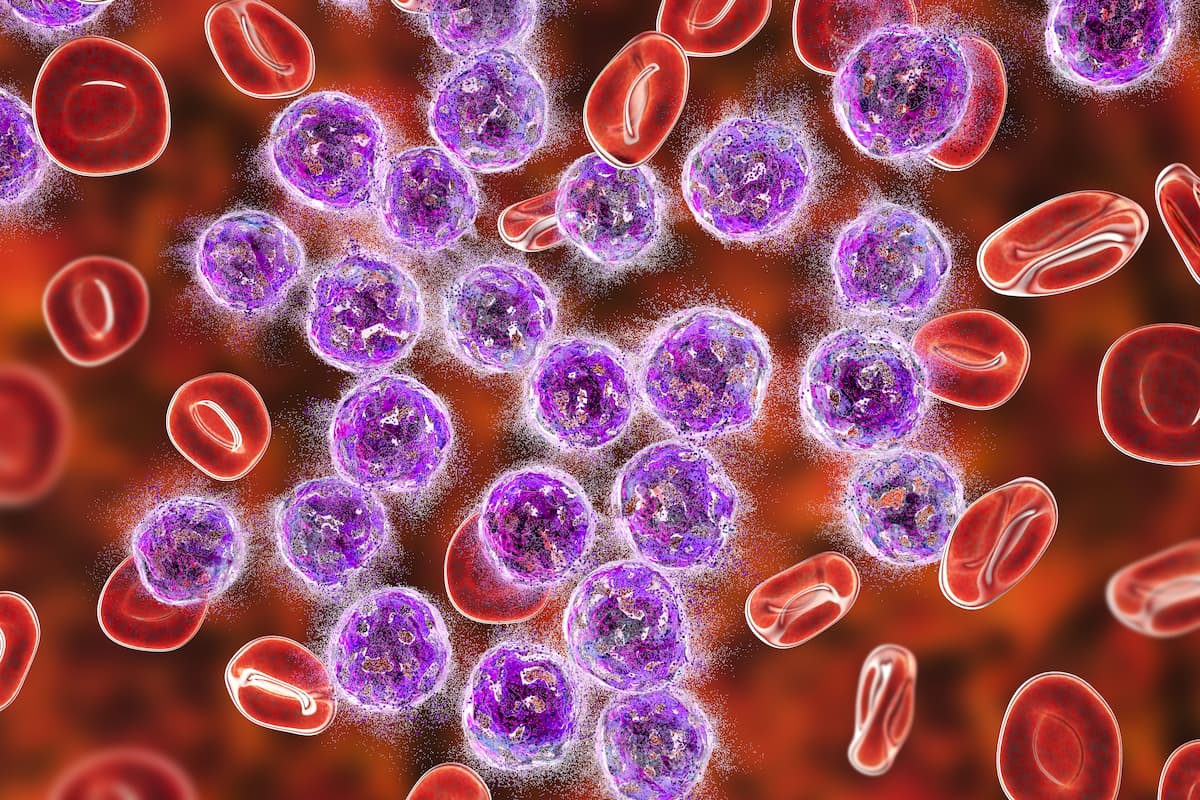
Basal ctDNA May Predict Treatment Outcomes in Follicular Lymphoma
Data from a prospective pilot study indicate that circulating tumor DNA may be a valuable prognostic biomarker in early-stage follicular lymphoma.
Higher basal circulating tumor DNA (ctDNA) levels correlated with a greater risk of progression and was predictive of treatment outcomes in a cohort of patients with follicular lymphoma, according to data from a prospective pilot study published in Clinical Cancer Research.
"These results suggest that detecting somatic mutations in pretreatment cfDNA is favored by lower response rates to first-line chemoimmunotherapy, a higher risk of early progression, and greater follicular lymphoma aggressiveness," according to the authors of a prospective study.
Of 411 diagnostic tissue samples, 300 contained basal cfDNA. Investigators noted that the mean number of alterations per cfDNA sample were significantly higher in patients who experienced progressive disease within 24 months or did not achieve a complete response (CR) vs those who did not progress at 24 months or who had a CR.
Moreover, the number of mutations present in basal cfDNA samples was associated with response and progression at 24-weeks in the follicular lymphoma cohort. When examining paired basal cell-free DNA (cfDNA) samples from 23 patients, investigators identified a mean of 18 (range, 11-29) alterations per sample in patients who experienced progression after 24 months vs a mean of 4.7 (range, 0-19) in those who didn’t (P = .0001).
Patients who didn’t experience a CR had a mean of 14.2 alterations (range, 3-29) vs a mean of 3.9 (range, 0-17) in those who did (P = .001). Moreover, basal ctDNA levels were significantly higher in patients without a CR than their counterparts (P = .02).
“Identifying patients at higher risk of [disease progression at 24 months] at diagnosis is a clinically relevant problem,” the investigators wrote. “These results suggest that detecting somatic mutations in pretreatment cfDNA is favored by lower response rates to first-line chemoimmunotherapy, a higher risk of early progression, and greater follicular lymphoma aggressiveness. From a different perspective, the nondetection of ctDNA in pretreatment plasma samples could be a biomarker of good prognosis.”
This prospective pilot study examined 100 plasma samples from 36 patients. Most were female (61%), 60 years of age or older (61%), and did not experience progression at 24 months (83%). Most patients had grade 2 disease (46%), with the remainder evenly split between grade I (27%) and grade IIIA (27%) disease. Exactly one-half of patients had extranodal involvement and a majority (57%) did not have bone marrow involvement.
Patients were treated with either rituximab (Rituxan; n = 3); cyclophosphamide, hydroxydaunorubicin, vincristine, and prednisolone (R-CHOP; n = 6); cyclophosphamide, vincristine, and prednisolone (R-CVP; n = 2), rituximab plus bendamustine (21 patients), or radiotherapy only (n = 1).
A wait and watch approach was employed for a further 5 patients at diagnosis, 2 of whom were subsequently treated when disease symptoms appeared.
First-line chemoimmunotherapy (CI) or radiotherapy achieved a CR in 23 patients, a partial response in 8, and no response in 1.
Half of the patient population was positive for high disease burden according to Groupe d’Etude des Lymphomes Folliculaires (GELF) criteria. All received treatment and 55.5% experienced a complete response. Of 12 patients with negative GELF criteria, 91.2% achieved a CR following treatment with radiotherapy or chemoimmunotherapy.
Pretreatment ctDNA levels were higher in patients who experienced progression at 24 months vs those who didn’t in both the GELF-negative (P = .04) and -positive (P = .004) groups.
Moreover, when assessing mid-treatment cfDNA, investigators found inferior event-free survival (EFS) in patients with at least 1 mutation—50% at 24 months—than in patients without mutations—90% (P = .008); investigators noted a somewhat low sensitivity. The same trend held true at the end of treatment.
“Plasma samples from patients with follicular lymphoma are expected to have around one tenth of the ctDNA calculated in patients with diffuse large B-cell lymphoma. This lesser amount of ctDNA reflects the smaller tumor volume, clinical stage, and more indolent characteristics of this type of lymphoma,” the investigators wrote. “Sensitivity would be improved by using larger plasma volumes and more sensitive methods, such as phased variant detection…. [T]he detection of somatic phased variants in cfDNA provides us with a promising tool for improving ctDNA detection sensitivity....”
The authors noted that further studies with larger cohort sizes are required to further support these findings and refine monitoring techniques.
Reference
Fernández-Miranda I, Pedrosa L, Llanos M, et al. Monitoring of circulating tumor DNA predicts response to treatment and early progression in follicular lymphoma: results of a prospective pilot study. Clin Cancer Res. 2023;29(1):209-220. doi:10.1158/1078-0432.CCR-22-1654
How Supportive Care Methods Can Improve Oncology Outcomes
Experts discussed supportive care and why it should be integrated into standard oncology care.