Best to Stage Esophageal Cancer After Neoadjuvant Chemo
The stage of esophageal adenocarcinomas after neoadjuvant chemotherapy is predictive of outcomes, rather than the stage determined prior to therapy.
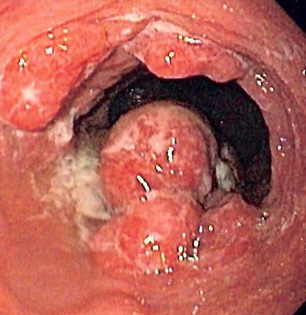
Endoscopic image of patient with esophageal adenocarcinoma; source: Wikimedia Commons
The stage of esophageal adenocarcinomas after neoadjuvant chemotherapy is significantly predictive of outcomes, rather than the stage determined prior to therapy, according to a new study. Restaging after the treatment can help clinicians more accurately and effectively decide on surgery or other courses of treatment.
“The absolute benefit of neoadjuvant chemotherapy remains relatively low,” wrote study authors led by Andrew R. Davies, MD, of St. Thomas’ Hospital in London, adding that only about 15% of esophageal cancer patients saw absolute improvements in survival. “Identification of these patients would represent significant clinical progress and could potentially herald patient-specific management.”
The group analyzed outcomes from 584 patients at two centers in London, 400 of whom (68%) received neoadjuvant chemotherapy. All patients were staged prior to therapy, which was compared with pathologic stage after surgical resection. Results were published online ahead of print in the Journal of Clinical Oncology.
Patients whose tumors were downstaged following chemotherapy (175 patients, 44%) had better survival compared to patients without any tumor response (P < .001). In fact, downstaging was found to be the strongest independent predictor of survival even after adjustment for patient age, tumor grade, clinical tumor stage, lymphovascular invasion, resection margin status, and surgical resection type; the hazard ratio for survival for downstaged patients was 0.43 (95% CI, 0.31-0.59).
The patients who were downstaged clearly benefited from some specifics of their response. They experienced lower rates of local recurrence than patients with no response (6% vs 13%; P = .030), as well as systemic recurrence (19% vs 29%; P = .027). They also had improved Mandard tumor regression scores (P < .001).
“Patients who had downstaging of their primary tumor after chemotherapy had survival comparable to that of patients with equivalent early-stage tumors who did not require chemotherapy,” the authors wrote. “Thus, tumor stage after neoadjuvant chemotherapy seems to be more important than initial stage at presentation in terms of assessing prognosis.” Specifically, they noted that this finding suggests advanced diagnostic procedures for staging such as PET-CT and MRI should be used for post-therapy staging rather than only at diagnosis. With better post-chemotherapy staging, treatments could potentially be tailored more specifically to individuals.
Study Details
The mean age of patients was 63 years, and most patients (86%) were men. The overall survival of the full cohort was 80% at 1 year and 45% at 5 years. Surgery consisted of transhiatal esophagectomy in 232 patients, and transthoracic esophagectomy in 353 patients. The most commonly used chemotherapy regimens were ECF (epirubicin, cisplatin, and fluorouracil 5FU), cisplatin and fluorouracil, and epirubicin, cisplatin, and capecitabine; those accounted for 96% of all patients.