Bone Marrow Microenvironment Could Offer Future Target in CML
Modulation of the bone marrow microenvironment with parathyroid hormone may be a feasible way to dramatically reduce counts of leukemia stem cells in chronic myeloid leukemia patients, according to new research in mice.
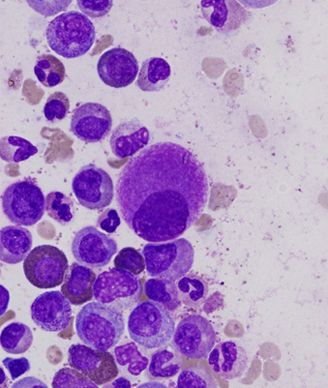
A small, hypolobated megakaryocyte in a bone marrow aspirate, typical of CML; source: Difu Wu, Wikimedia Commons
Modulation of the bone marrow microenvironment with parathyroid hormone (PTH) may be a feasible way to dramatically reduce counts of leukemia stem cells in chronic myeloid leukemia (CML) patients, according to new research in mice. Reducing leukemia stem cells (LSCs) is a required step on the path to a true cure for the disease.
“Like their normal hematopoietic stem cell counterparts, leukemia stem cells in CML and acute myeloid leukemia (AML) are presumed to reside in specific niches in the bone marrow microenvironment and may be the cause of relapse following chemotherapy,” wrote investigators led by Daniela S. Krause, MD, PhD, of Massachusetts General Hospital in Boston. The study was published in Nature Medicine.
Krause and her colleagues tested transgenic mice bred to have osteoblastic cell-specific expression of an active receptor for PTH and compared them with wild-type mice as recipients of retroviral transduction-transplantation of myeloproliferative neoplasia, a condition that resembles CML. In the mice where the PTH receptor was modified, the cumulative mortality due to that CML-like myeloproliferative neoplasia was significantly decreased (P < .001) and the overall survival of the mice was prolonged (P = .002). Treatment with PTH also yielded a 15-fold reduction in frequency of LSCs in the bone marrow (P = .0006).
In contrast, mice treated in the same way showed an enhancement of oncogene-induced AML. The difference in response suggests that the specific niches where LSCs reside in CML and AML are distinct. The mechanism by which PTH offers a benefit in CML appears to be via release from the microenvironment of transforming growth factor-Ã1 (TGF-Ã1); the protein exhibits a suppressive effect on CML stem cells.
The investigators also injected total bone marrow cells from seven human untreated chronic phase CML patients into mice pretreated with either saline or PTH. PTH treatment was significantly associated with a decrease in leukemic engraftment (P = .049), a finding that the authors wrote provides support for testing PTH in human subjects with CML.
“Our results suggest that targeting the hematopoietic microenvironment through [parathyroid hormone] may render it hostile for CML cells, raising the possibility of altering the tumor microenvironment as potentially complementary approach to tumor cell-specific therapeutics,” they concluded.