BRAF/MEK Combo Improved Outcomes in Melanoma
Combining BRAF and MEK inhibitors resulted in better response, PFS, and overall survival compared with a BRAF inhibitor alone in BRAF-positive melanoma patients, according to results presented at the 2014 ESMO Congress.
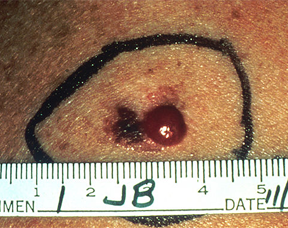
Advanced malignant melanoma.
Combining a BRAF inhibitor with a MEK inhibitor resulted in better progression-free survival, response, and overall survival rates than those seen with the use of a BRAF inhibitor alone in patients with BRAFV600-positive melanoma, according to the results of two phase III studies presented at the 2014 European Society for Medical Oncology (ESMO) Congress.
The combination of a BRAF and MEK inhibitor was thought to be able to improve outcomes in patients with BRAF-positive melanoma by delaying BRAF inhibitor resistance eventually seen in most patients. Prior research had shown that vemurafenib, a BRAF inhibitor, and cobimetinib, a MEK inhibitor, could be given concomitantly, and had high rates of tumor shrinkage.
In the first phase III study (Abstract 5LBA_PR), Grant McArthur, MD, head of the Cancer Therapeutics Program at the Peter MacCallum Cancer Centre, Melbourne, Australia, and colleagues enrolled 495 patients with previously untreated, BRAF-positive unresectable locally advanced or metastatic disease. Patients were randomly assigned to vemurafenib 960 mg twice a day for 28 days, plus cobimetinib or placebo at 60 mg daily from day 1 to 21.
Treatment with the combination regimen results in a significant improvement in progression-free survival compared with treatment with vemurafenib alone. The median progression-free survival was 9.9 months for patients assigned the combination compared with 6.2 months for those assigned the BRAF inhibitor alone (HR = 0.51; 95% CI, 0.39-0.68; P < .0001). Patients assigned the combination also had significantly improved response rates (68% vs 45%; P < .0001).
“We anticipate that the combination of a BRAF and MEK inhibitor will become a new standard treatment for advanced BRAF-mutant melanoma,” McArthur said in a prepared statement. “The data lay the foundation for the addition of treatments either in sequence or in further combination to obtain even better results.”
The overall survival analysis did not cross the prespecified boundary for significance.
Patients assigned to the BRAF/MEK combination had a higher incidence of grade 3 or higher adverse events (65% vs 59%); however, this difference did not result in a significantly different rate of drug discontinuation.
In the second study (4LBA_PR), Caroline Robert, MD, head of dermatology at the Institute Gustave Roussy, Paris, France, and colleagues randomly assigned patients to BRAF inhibitor dabrafenib 150 mg twice daily plus MEK inhibitor trametinib 2 mg once daily (n = 352) or BRAF inhibitor vemurafenib 960 mg twice daily monotherapy (n = 352). Patients were aged 18 years or older and had unresectable locally advanced or metastatic BRAFV600E/K positive melanoma.
The study was stopped early at an interim analysis that showed a 31% improvement in overall survival in patients assigned to the combination therapy. Patients assigned to a BRAF/MEK inhibitor combination also had a 44% reduction in the risk of disease progression compared with patients assigned vemurafenib monotherapy. The median progression-free survival was 11.4 months for patients assigned the combination compared with 7.3 months for monotherapy.