Breast Cancer Cryoablation May Be Safer Alternative to Invasive Surgery in Select Patients
Retrospective analysis found that cryoablation was associated with infrequent AEs and low recurrence rates among patients with breast cancer.
Retrospective analysis found that cryoablation was associated with infrequent AEs and low recurrence rates among patients with breast cancer.
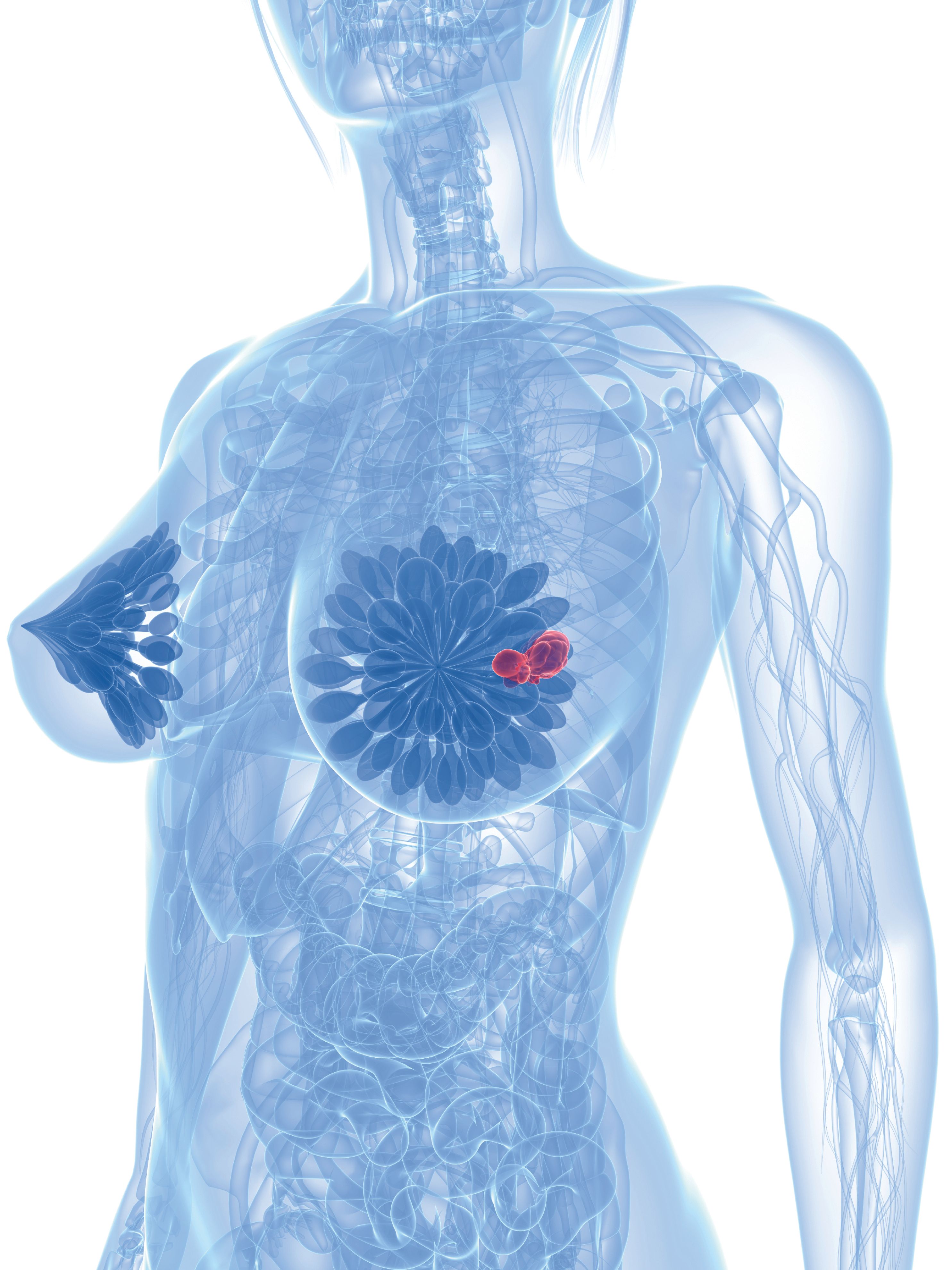
Cryoablation may be a viable alternative to surgery for patients with primary breast cancer who have unfavorable patient or tumor characteristics or are poor surgical candidates, according to findings from a retrospective study published in the American Journal of Roentgenology.
Results from the study found that of 112 patients included for analysis who underwent cryoablation, 110 (98.2%) had technically successful procedures. At a median follow-up of 2.0 years (95% CI, 1.7-2.2), ipsilateral breast tumor recurrence (IBTR) occurred in 12 of 110 patients (10.9%) who had successful procedures, including 5 with new primary disease. Cumulative IBTR incidence was at 1, 2, and 3 years was 5.3% (SE = 0.02%), 12.2% (SE = 0.04%), and 18.2% (SE = 0.06%), respectively, when accounting for death.
Grade 1 adverse events (AEs) occurred in 7 of 112 (6.3%) patients; no AEs greater than grade 1 occurred.
“In patients with breast cancer who underwent cryoablation with locally curative intent despite being ineligible for cryoablation clinical trials, such treatment had a low frequency of AEs and a high frequency of procedural technical success. The frequency of IBTR was higher than previously reported for prospective clinical trials. Nonetheless, in select individuals with unfavorable patient or tumor characteristics, cryoablation remains a safe alternative to surgery that has overall good outcomes. These findings may be particularly relevant in patients who are also poor surgical candidates due to comorbidities,” wrote Karim Oueidat, MD, internal medicine resident at the American University of Beirut in Beirut, Lebanon, with study coinvestigators in the publication.
The study initially identified 144 patients with primary breast cancer who underwent cryoablation between January 1, 2000 and August 26, 2021.Patients eligible for prospective clinical trials (n = 10), who underwent cryoablation with palliative intent (n = 2), who had multifocal or multicentric disease (n = 7), and those with no imaging follow-up before the end of study period (n = 13) were excluded from the final sample; a total of 112 patients remained.
Grade 1, 2, and 3 tumors were assessed in 61 (54.5%), 40 (35.7%), and 11 (9.8%) patients, respectively. ER-positive, PR-positive, or HER2-negative hormone receptor status was observed in 87 patients (77.7%) and triple-negative status was observed in 10 patients (8.9%).
Performance of cryoablation was done in 7 centers by 7 radiologists under ultrasound guidance in the outpatient setting. Procedures aimed to center the lesion within the ice and encapsulate it within at least 0.5 to 1.0 cm beyond all tumor margins. Freeze-thaw cycles occurred 2 times and typically included freezes with intervening passive thawing both at 5 to 10-minute intervals.
Between preablation lesion biopsy and cryoablation, the median time was 49.5 days (IQR, 36-100). Median freeze time duration was 14 minutes (IQR, 12-16) with median long- and short-axis diameters of maximum formed ice ball were 5.0 cm (IQR, 4.4-5.5) and 3.6 cm (IQR, 3.0-4.0), respectively. Intraprocedural hydrodisplacement occurred in 104 (92.9%) procedures, with a median volume of 50 mL (IQR, 30-100 mL).
The 2 treatment failures included 1 occurrence due to a hematoma-caused ice propagation and 1 due to insufficient liquid nitrogen availability; none were due to evidence of residual disease on first imaging follow-up.
Of 110 patients in the safety analysis, 7 died, including 1 from a cancer-related death and another who had IBTR classified as a non-cancer-related death. At 1, 2, and 3 years, the likelihood of death following cryoablation was 3.3% (SE = 0.02%), 6.9% (SE = 0.03%), and 19.9% (SE = 0.09%), respectively.
Reference
Oueidat K, Baird GL, Barclay-White B, et al. Cryoablation of primary breast cancer in patients ineligible for clinical trials: a multiinstitutional study. Am J Roentgenol. Published online July 10, 2024. doi:10.2214/AJR.24.31392