Since most patients with Hodgkin lymphoma survive their disease, long-term issues such as development of second primary malignancies arise, especially in patients treated with multimodal therapy including radiation therapy plus chemotherapy. The risk of breast cancer is significantly elevated in women exposed to high-dose ionizing radiation to the chest before age 40. The case of a 48-year-old patient with a lump in her right breast is presented as a clinical scenario in this article. We review available strategies for screening and risk reduction through chemoprevention or risk-reducing surgery, as well as challenges for management of breast cancer in patients with prior exposure to radiation for Hodgkin lymphoma. The Children’s Oncology Group clinical practice guidelines for long-term follow-up care of pediatric cancer survivors provide recommendations that have been endorsed by American and European oncologists.
Clinical Scenario
A 48-year-old premenopausal woman presented with a 3-cm lump in her right breast. Her history included menarche at the age of 14. At the age of 28 she was diagnosed with stage I Hodgkin lymphoma, nodular sclerosis subtype, involving the left cervical lymph nodes. Imaging demonstrated no mediastinal or subdiaphragmatic disease. Following a staging laparotomy with sampling of para-aortic lymph nodes and splenectomy, no tumor involvement below the diaphragm was identified. She was treated with definitive mantle radiation therapy (RT) alone, to a dose of 35 Gy. She subsequently developed hypothyroidism and gastroesophageal reflux disease. At the age of 44 she underwent in vitro fertilization following clomiphene due to infertility, and at age 45 delivered a healthy girl.
She was concerned about her risk of developing breast cancer following RT to her chest, and was considering prophylactic mastectomy. It was during this period that she discovered the lump in her right breast.
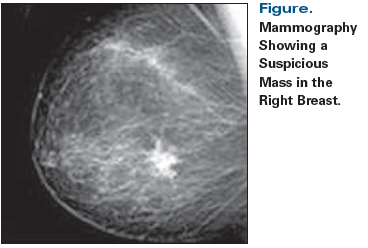
Mammography (Figure) showed a 3-cm spiculated mass at 9 o’clock in the right breast. Biopsy was positive for a grade 3 invasive ductal carcinoma that was estrogen receptor (ER)-positive (69%) and progesterone receptor (PR)-positive (68%), but negative for human epidermal growth factor receptor 2 (HER2) overexpression by immunohistochemistry. The Ki-67 index was positive in 67% of tumor cells. Her examination was negative for axillary lymph node involvement. The patient underwent bilateral mastectomy with sentinel lymph node biopsy and reconstruction. The pathology report showed a 3-cm primary tumor in the right breast, and metastatic carcinoma involving 2 out of 5 right axillary lymph nodes. She received adjuvant chemotherapy with dose-dense AC-T (doxorubicin, cyclophosphamide, and paclitaxel). She later had a hysterectomy with bilateral salpingo-oophorectomy, and started adjuvant anastrozole. She did not receive adjuvant chest wall and regional nodal radiation, given her prior course of treatment for Hodgkin lymphoma.
Two years later, she developed multiple biopsy-proven bone and nodal breast cancer metastases in cervical, mediastinal, and hilar nodes. Antiresorptive therapy with denosumab was administered. She was first treated with fulvestrant, and upon progression 9 months later, was switched to exemestane and everolimus, with stable disease for now.
The critical questions in this patient’s care include:
1) What is the risk of developing breast cancer in women with prior RT to the chest?
2) Is there a role for risk-reducing endocrine therapy in patients with prior RT to the chest?
3) Is there a role for risk-reducing surgery in patients with prior RT to the chest?
4) What are the challenges of treating breast cancer in a patient with prior exposure to chest radiation?
Incidence and Prevalence of Breast Cancer Following RT
Since the majority of children and adolescents succeed in their fight with cancer, lifelong awareness about long-term health issues, such as second primary tumors, is warranted. Women exposed to chest radiation as children, adolescents, or young adults are at a significantly increased risk for developing breast cancer over time.[1-6] Radiation is known to increase risk of secondary malignancies in exposed tissue. Radiation-induced breast cancer has been identified in adult survivors of various childhood cancers treated with RT to the chest, such as Hodgkin lymphoma, non-Hodgkin lymphoma, bone tumors, Wilms tumor, neuroblastoma, and soft-tissue sarcoma.[7,8] The risk of developing breast cancer correlates with the radiation dose to the exposed breast tissue, the age of the patient at the time of radiation treatment, and the amount of time since radiation exposure.[8-12] The risk of radiation-induced breast cancer increases above the risk of the general population about 8 years after RT and does not appear to plateau over time.[8-12] A recent population-based study from the Netherlands evaluating 1,055 patients treated for Hodgkin lymphoma between 1965 and 2000 demonstrated a 16% 30-year cumulative incidence rate of breast cancer (whether or not they received RT).[13] Compared with patients who did not receive chest irradiation, the incidence of breast cancer was 4.2 times greater with the use of mantle field irradiation, and 1.5 to 1.7 times with other (smaller) radiation fields.
Alhough women with this unique treatment-related exposure face an elevated risk of a breast cancer diagnosis approximately 15 to 20 years earlier than their age-matched peers without such exposure, to date there is little evidence that the characteristics of the breast cancer itself are any different from those of breast cancer that develops in older women, except that there appears to be a higher incidence of bilateral breast cancer.[8] In studies that have reported on diagnostic characteristics of breast cancers occurring in women with a history of radiation exposure, most of which are small cohort studies or summarized in a 2010 systematic review,[8] the breast cancers tended to be intraductal, with a prevalence of hormone receptor expression similar to that described in the general population, although one population-based study published later in 2012 reported a higher incidence of hormone receptor–negative breast cancer.[12] Five-year breast cancer survival rates among women with early-stage breast cancer secondary to RT exposure are also similar to rates described in the general population.[8] The presentation of the breast cancer described in this case is consistent with a radiation-induced breast cancer related to past Hodgkin lymphoma treatment.
Surveillance Strategies
The increased risk of breast cancer in adult women with a history of pediatric or young adult exposure to high-dose chest radiation parallels the risk faced by those with an inherited mutation in the BRCA1 and BRCA2 genes,[13-17] with a cumulative incidence rate approaching 20% by the age of 40 to 45.[8] This is significantly higher compared with rates in young women in the general population, in whom the cumulative incidence rate of breast cancer by 45 years of age is only 1% to 2%.[8] Because of this high risk, women exposed to high-dose chest radiation as children or young adults benefit from long-term breast cancer surveillance.
In 2004, the Children’s Oncology Group (COG) developed clinical practice guidelines to direct follow-up care for pediatric cancer survivors.[18] The COG Long-Term Follow-Up (LTFU) Guidelines are publicly available at www.survivorshipguidelines.org. These guidelines were originally based on expert consensus, with evidence derived from populations with similar cumulative risk, such as those with hereditary mutations, because specific evidence was lacking in the pediatric and young adult cancer survivor population. The COG LTFU Guidelines address the increased risk of breast cancer necessitating screening in patients treated with RT to the chest, axilla, and thorax with doses of 20 Gy or more. Patients treated with mini-mantle, extended-mantle, or mantle radiation fields (like the patient in the clinical scenario) fall into this category. COG recommends the following breast cancer screening measures:
1) Clinical breast exam yearly starting from puberty to the age of 25, then every 6 months.
2) Mammography and breast MRI yearly starting from the age of 25 or 8 years after RT, whichever occurs later.
3) Patient education on self-breast exams, with subsequent self-breast exams performed monthly beginning at puberty.
Importantly, the use of breast MRI as an adjunct to screening mammography in women exposed to chest radiation has been subsequently endorsed by the American Cancer Society[19] and validated in prospective studies demonstrating increased specificity and sensitivity for mammography and MRI together in detecting breast cancer in survivors of Hodgkin lymphoma.[20,21] These recommendations have been incorporated into recent National Comprehensive Cancer Network (NCCN) guidelines for the follow-up of patients treated for Hodgkin lymphoma.[22]
The COG LTFU Guidelines acknowledge the fact that higher radiation doses, exposure to RT at an earlier age, and longer time since exposure are associated with the increased risk of breast cancer.[18] At the same time, exposure to alkylating agents or pelvic radiation leading to premature ovarian failure and early menopause may decrease the risk of breast cancer, presumably by reducing exposure of radiation-damaged breast cells to the stimulating effect of ovarian hormones. However, in the absence of prospective data, the surveillance guidelines do not differ in the subgroup of patients previously exposed to alkylating agents or pelvic radiation.
In 2013, an international multidisciplinary panel of experts from Europe and North America (International Guideline Harmonization Group) developed comprehensive recommendations for breast cancer surveillance for female survivors of childhood, adolescent, and young adult cancers who received chest radiation.[23] These recommendations summarized the most recent evidence available worldwide, and harmonized screening recommendations between Europe and the United States based on guidelines previously developed by COG, the Dutch Childhood Oncology Group, the Scottish Intercollegiate Guidelines Network, and the UK Children’s Cancer and Leukaemia Group.[24] The harmonization guidelines concur with screening measures suggested by COG, and confirm that women who received chest radiation with a dose of 20 Gy or more before the age of 30 years are at the highest risk for developing breast cancer. Additionally, the harmonization guidelines underscore that there is no clear cutoff for a safe radiation dose.[23] Individuals who received radiation with potential impact to the breast (including chest wall, whole lung, mediastinum, axillary, subtotal lymphoid, upper abdominal, or total body irradiation) when they were under the age of 30 may have increased risk of breast cancer, even if the radiation dose to the breast was below 20 Gy. Breast cancer screening should be considered for all of these individuals. The strength of this recommendation is based on chest radiation dose categories: strong recommendation for screening at a high dose (≥ 20 Gy), moderate recommendation for a moderate dose (10–19 Gy), and weak recommendation for a low dose (1–9 Gy). Odds ratios for the development of breast cancer in women who were given chest radiation with doses below 10 Gy and 10–19 Gy are about 1.9 and 6.5, respectively, compared with the general population. Medical decision making for these patients should be based on the clinical scenario; patient preferences; and relevant risk factors, such as breast density, current age, and family history.[21] It is important to note that the Gail model is not an appropriate breast cancer risk assessment tool for women who received prior thoracic radiation.
Another important point from the harmonization guidelines is that, although definitive studies with long-term follow-up are lacking, follow-up of women up to age 50 years showed that the risk of radiation-induced breast cancer does not seem to diminish with age. The biologic mechanisms of radiation-induced breast tissue apoptosis and carcinogenesis suggest that the cumulative incidence of breast cancer will continue to increase with age, and that the excess risk will remain substantially elevated. For this reason, continuous surveillance of female survivors of childhood and young adult cancers is reasonable even after 50 years, pending availability of further data.
Data on a cohort of 40,000 women demonstrate that the risk of a second breast cancer developing in women treated with radiation for primary breast cancer is limited.[25] However, one of the reasons for this may be the older age of these women at the time of radiation exposure, as compared with women treated with RT for Hodgkin lymphoma.
It is worth noting that for many women with a secondary, radiation-induced breast cancer following a primary cancer, treatment for their breast cancer may need to be modified due to other cumulative treatment exposures they have received in the past for their primary cancer. These patients may not be able to receive additional chest wall radiation because of prior RT to the chest, or may have limitations on cumulative doses of chemotherapeutic agents. Disease-free and overall survival for these patients may be negatively impacted as a result of these factors, especially if they present with advanced-stage breast cancer. This, again, underscores the importance of prevention, surveillance, and early detection of secondary breast cancer in this patient population.[26]
However, the best surveillance guidelines are only helpful if physicians and patients are aware of them. The patient in this case was not undergoing high-risk screening mammography or breast MRI prior to diagnosis. It is not known what recommendations had or had not been provided after her Hodgkin lymphoma therapy was completed.[1] An observational study demonstrated that many adult survivors of childhood cancer are unaware of their risks for secondary breast cancer after chest irradiation, and a large proportion of these patients miss the opportunities for early breast cancer screening.[21] Many of them believe they do not need long-term follow-up and screening because they are cured from their childhood cancer. Transition of childhood and young adult cancer survivors between pediatric and adult clinics may lead to loss of follow-up and missed screening opportunities for radiation-induced secondary cancers. Patient education and communication between pediatric and adult oncologists and primary care providers create opportunities to improve outcomes and save lives. Detailed diagnostic and treatment information regarding primary childhood, adolescent, or young adult cancer is critical not only for the pediatric and adult oncology teams, but for all healthcare providers, including primary care providers, so that they can counsel individual patients on their long-term health risks.
Pharmacologic Risk-Reducing Strategies
In addition to general health promotion counseling and modifications of traditional behaviors known to be involved in the development of cancer in general (obesity, smoking, heavy alcohol intake, sedentary lifestyle, diet high in saturated fat), pharmacologic risk-reducing strategies play an important role in mitigating radiation-induced breast cancer risk. Although no clinical trial to date has addressed the efficacy of breast cancer chemoprevention specifically in childhood and young adult cancer survivors exposed to chest wall radiation, the selective estrogen receptor modulators (SERMs) tamoxifen and raloxifene should be considered, based on extrapolation of data from other high-risk populations. Tamoxifen and raloxifene have been approved by the US Food and Drug Administration (FDA) for primary breast cancer prevention in pre- and postmenopausal women, respectively, at high risk for breast cancer. Evidence for the preventive benefits of SERMs has been shown only in high-risk women who are 35 years of age and older; benefits in younger women are unknown. Tamoxifen increases a woman’s fertility during therapy and is contraindicated during pregnancy,[27] so detailed discussion of reproductive desires and contraception are indicated before commencing therapy. A meta-analysis of individual participant data from 9 prevention trials comparing 5 years of SERMs with placebo showed an overall 38% reduction in the incidence of invasive breast cancer (hazard ratio [HR], 0.62 [95% CI, 0.56–0.69]).[28]
In our case scenario, the patient had a premenopausal breast cancer diagnosis, and the option of tamoxifen prevention could have been used. The US Preventive Services Task Force, the American Society of Clinical Oncology, and NCCN guidelines recommend tamoxifen for primary breast cancer prevention in women age 35 years and older at high risk for breast cancer.[29-31] Tamoxifen gained FDA approval for breast cancer prevention based on the results of the National Surgical Adjuvant Breast and Bowel Project P-1 clinical trial.[32] In this trial, women who were 60 years of age or older, or 35 to 59 years of age with a 5-year predicted risk of breast cancer of at least 1.66%, or who were any age and had a history of lobular carcinoma in situ, were randomly assigned to receive placebo (n = 6,707) or tamoxifen at 20 mg per day (n = 6,681) for 5 years. Overall, tamoxifen reduced the risk of invasive breast cancer by 49%, with cumulative incidence through 69 months of follow-up of 43.4 vs 22.0 per 1,000 women in the placebo and tamoxifen groups, respectively. Importantly, the occurrence of ER-positive tumors was reduced by 69%, but no difference in the occurrence of ER-negative tumors was seen. Additionally, tamoxifen reduced the risk of ductal carcinoma in situ by 50%. Tamoxifen was beneficial for bone health in postmenopausal women: a reduction in hip, radius, and spine fractures was observed. The rate of endometrial cancer was increased in the tamoxifen group (relative risk [RR], 2.53 [95% CI, 1.35–4.97]), as were the rates of stroke, pulmonary embolism, and deep vein thrombosis. However, these complications occurred predominantly in women aged 50 or older.[32] A 2012 meta-analysis confirmed a very low risk of these complications in women under 50 years of age, with an RR of 1.19 (95% CI, 0.53–2.65) for endometrial cancer, 2.30 (95% CI, 1.23–4.31) for deep vein thrombosis in the active phase of treatment, and 1.16 (95% CI, 0.55–2.43) for pulmonary embolism.[33] Also, tamoxifen is not protective of bone health in premenopausal women.
The International Breast Cancer Intervention Study I provided long-term follow-up of women exposed to 5 years of tamoxifen for primary breast cancer prevention.[34] In this trial, 7,154 women were randomly assigned to tamoxifen (n = 3,579) or placebo (n = 3,575). After a median follow-up of 16 years, the incidence rate of breast cancer was 7% in the tamoxifen group vs 9.8% in the placebo group (HR, 0.71 [95% CI, 0.60–0.83]). Importantly, the risk of developing breast cancer was similar between years 0 and 10 (HR, 0.72 [95% CI, 0.59–0.88]) and after 10 years (HR, 0.69 [95% CI, 0.53–0.91]). These results showed that tamoxifen offers a very long period of protection after treatment cessation, persisting beyond 10 years post-treatment, and this substantially improves the benefit-harm ratio of tamoxifen for breast cancer prevention.[34] The durable long-term protective effect of tamoxifen was confirmed in several European clinical trials.[35,36] These studies were not powered to detect a survival advantage, and consequently, a breast cancer–specific or all-cause mortality benefit was not found for tamoxifen prophylaxis.[28,32,37] To date, tamoxifen remains the primary option for chemoprevention in premenopausal women.
Unfortunately, pharmacologic breast cancer risk-reduction therapy is greatly underutilized.[37,38] Despite multiple publications highlighting the role of chemoprevention in high-risk patients, general acceptance of it is low,[38] and both patient and provider factors are thought to play a role. Among providers, barriers for prescribing medications for primary breast cancer prevention include inadequate training in risk assessment, lack of reimbursement for prevention counseling, and the lack of easily accessible and user-friendly prediction tools for risk-benefit ratios.[39] Patient-related factors include inadequate education about breast cancer risk, the paucity of information that accurately conveys the risks and benefits of preventive medications,[39] and concerns about medication side effects. A recent study from Moffitt Cancer Center showed that only 54% of women at increased risk for breast cancer accepted a recommendation for chemoprevention and began therapy, and approximately 40% of them were not able to complete 5 years of therapy because of side effects.[38]
TO PUT THAT INTO CONTEXT
Kathleen Horst, MD[[{"type":"media","view_mode":"media_crop","fid":"55121","attributes":{"alt":"","class":"media-image","id":"media_crop_8702677897544","media_crop_h":"0","media_crop_image_style":"-1","media_crop_instance":"6901","media_crop_rotate":"0","media_crop_scale_h":"0","media_crop_scale_w":"0","media_crop_w":"0","media_crop_x":"0","media_crop_y":"0","style":"height: 174px; width: 144px;","title":" ","typeof":"foaf:Image"}}]]Sarah S. Donaldson, MD, Department of Radiation Oncology
Stanford University Cancer Center
Stanford, CaliforniaHow Do We Move Forward With Treating Hodgkin Lymphoma Survivors Who Develop Breast Cancer?When Dr. Henry Kaplan began treating patients with Hodgkin disease (now Hodgkin lymphoma) in the early 1960s, it was unclear whether cure was possible for a disease that was, at that time, universally fatal. Astoundingly, the randomized trials that Kaplan and his team conducted led to disease-free and overall survival rates of more than 90%. The challenge that now remains is to build on Dr. Kaplan’s success by continuing to maintain high cure rates while striving to reduce or prevent the long-term side effects of treatment. In particular, this review discusses the risk and challenges of secondary breast cancer.The reported risk of developing breast cancer after successful treatment of Hodgkin lymphoma is based upon treatment regimens designed and delivered 2 to 4 decades ago, a time when the goal was to improve the chemotherapy and radiotherapy protocols for optimal cure. Since then, there have been significant changes in radiation doses, fields, and techniques, such that the risk of carcinogenesis related to these more contemporary treatments will likely be different from what we have previously witnessed.Clinical practice will continue to evolve with improved patient and provider education about risks, more routine incorporation of breast MRI into screening programs for early detection, and refinement of risk-based treatments for both Hodgkin lymphoma and breast cancer.What Can We Expect in the Future? We still need to better understand which patients need radiotherapy for Hodgkin lymphoma and which patients are at highest risk for developing breast cancer. We also need to better define the impact of genetic predisposition and the relevance of new genes, including variants of uncertain significance. It will be important for future research to address the mechanism of radiation-associated carcinogenesis in order to identify potential targets for prevention and treatment of these cancers.In the future, treatment of lymphoma, as well as breast cancer prevention strategies, will continue to change and progress with the rapidly evolving technical advances in molecular identification of responsible genes, the development of new targeted agents, and further advances in radiotherapy precision.
Further complicating chemoprevention utilization in this unique population is the fact that the pivotal studies investigating anti-endocrine therapies for breast cancer prevention did not include women who received chest radiation for Hodgkin lymphoma. Thus, there are actually few direct data to confirm that similar benefits exist in this setting, although most oncologists presume the benefit would be similar. In addition, women treated for Hodgkin lymphoma are most often in their second to fourth decade of life at the time of treatment, and therefore are at a high risk for breast cancer at a very young age, beginning 7 to 10 years after irradiation. Many of these women have not yet considered or completed childbearing, and therefore are not ready to make a treatment decision that could potentially interfere with family planning.
A phase II randomized placebo-controlled trial is underway to evaluate the use of low-dose tamoxifen for young female survivors of childhood and young adult cancers who are at increased risk for breast cancer as a result of past exposure to chest radiation (ClinicalTrials.gov identifier: NCT01196936). This multisite study led by investigators at the University of Alabama, Birmingham will evaluate surrogate endpoint biomarkers of breast cancer risk-such as mammographic breast density, breast cytomorphology and proliferative index, sex steroid hormones, and insulin growth factors-after 2 years of therapy with 5-mg tamoxifen PO daily or placebo. This is the only currently ongoing trial investigating the use of medical therapy in reducing the risk of radiation-induced breast cancer.
Given the significantly increased risk of breast cancer in women exposed to chest radiation, these patients could greatly benefit from pharmacologic breast cancer prevention, and it could certainly be recommended, based on extrapolation of data from other high-risk populations. To date, clinical trials specific to the growing population of childhood and young adult cancer survivors are lacking, and this is a very important area for future research.
Surgical Risk-Reducing Strategies
Prophylactic bilateral mastectomy is associated with a > 95% reduction in the incidence of breast cancer in high-risk patients.[40] Women previously treated for Hodgkin lymphoma experience a 5.6-fold increased breast cancer risk when compared with the general population,[41] but performing bilateral mastectomy in women with a history of RT for Hodgkin lymphoma is controversial. When assessing these patients’ breast cancer risk, detailed information on their treatment history is critical to determine the benefit of prophylactic surgery.
The dose of radiation administered, as well as the volume of breast tissue exposed to radiation, directly correlate to a patient’s risk of breast cancer.[31] Treatment changes over the last 20 years favor an anticipated decreased breast cancer risk for women treated during this time period. Mantle field irradiation, which was standard treatment in the 1970s through the 1990s, is associated with an 8-fold increase in a woman’s breast cancer risk. Since the 1990s, however, radiation fields have become smaller as combined-modality therapy (combination chemotherapy and more limited RT) has become the standard therapy for early-stage disease.[42] Similarly, RT doses have decreased from approximately 40 Gy in the setting of single-modality definitive treatment to 20 to 30 Gy in the setting of combined-modality therapy.[42,43] Current RT guidelines state that radiotherapy should be directed to only initially involved sites of disease, and that postchemotherapy volumes should be utilized for treatment planning.[44] Thus, women treated in more recent years with limited radiation fields at lower doses are anticipated to have a lower risk of breast cancer than in the past. A recent report from the Netherlands documented a 63% relative reduction in breast cancer incidence for women treated to the mediastinum without inclusion of the axilla compared with those treated with full-mantle irradiation.[13] Nevertheless, since Hodgkin lymphoma involves the mediastinum in approximately 80% of patients, RT directed to nodal disease at this site will continue to place breast tissue at risk.
The duration of intact ovarian function after therapy also impacts breast cancer incidence. Treatment for Hodgkin lymphoma may involve alkylating chemotherapy and/or pelvic radiation, both of which adversely affect ovarian function. Patients 21 years old or younger who are treated for Hodgkin lymphoma have shown a 26% lifetime incidence rate of breast cancer, whereas women treated at 41 years of age or older do not show an increased risk of breast cancer.[2] These older patients tend to undergo menopause soon after therapy, whereas younger patients have many more years with intact ovarian function, thus increasing their future risk of breast cancer.
NCCN guidelines recommend that women with a history of thoracic radiation administered before the age of 30 should begin aggressive surveillance approximately 8 to 10 years after the radiation is administered.[22] The recommended surveillance includes biannual clinical exams and annual MRIs with mammograms. Prophylactic mastectomies should be discussed and can be offered to high-risk patients at the time of surveillance. Sentinel lymph node biopsy can be omitted if there are no concerning lesions on imaging. The reconstruction options depend on the degree of chest wall radiation changes. Patients with minimal skin changes who received radiation more than 10 years prior may be considered for immediate tissue expander–based reconstruction. Another option is autologous flap reconstruction.
The patient in the clinical scenario was at a considerable risk for developing breast cancer given her history of mantle field irradiation administered at the age of 28 years. She met the guidelines for an aggressive screening protocol and the option of prophylactic surgery.
Challenges of Treating Breast Cancer in a Patient With Prior Exposure to Chest RT
What is the phenotype of breast cancer following prior irradiation?
Limited data are available comparing breast cancer characteristics and treatment outcomes for patients who have a history of RT for Hodgkin lymphoma with those who do not have a history of prior RT. Elkin et al reported on 253 patients at multiple institutions in North America who were diagnosed with breast cancer following RT for Hodgkin lymphoma.[45] Survivors of Hodgkin lymphoma were more likely to be diagnosed with early-stage, node-negative disease when compared with patients with sporadic breast cancer matched by age, race, and year of breast cancer diagnosis.[45] The median age of breast cancer diagnosis in Hodgkin lymphoma survivors in this cohort was 42 years, which is significantly younger than the median age at breast cancer diagnosis in the United States (approximately 60 years).[46]
Breast cancers diagnosed in Hodgkin lymphoma survivors were hormone receptor–positive in 44% of cases compared with 50% in age-matched controls.[45] Data regarding HER2 status are lacking in this and other cohort studies, because of the year of diagnosis and lack of uniform HER2 testing. This study is unique in comparing Hodgkin lymphoma survivors who develop breast cancer to age-matched controls, and shows that the breast cancer phenotype is similar in these young women regardless of prior exposure to RT.
Is there any relationship between prior irradiation and sensitivity/resistance to hormone therapy?
The relationship between prior radiation and sensitivity of radiation-induced breast cancers to anti-endocrine therapy has not been directly addressed. Based on circumstantial evidence, the expectation is that, biologically, these tumors would demonstrate the same sensitivity as non–radiation-related breast cancer. Ovarian suppression or early ovarian function loss have been demonstrated to substantially decrease the risk of developing a radiation-induced breast cancer.[47] The effect was most prominent in patients who lost ovarian function within 10 years of receiving radiation. This observation seems to point to a mechanism similar to the alterations in DNA repair mechanisms in patients with BRCA mutations who have a similar and large degree of risk reduction.[48] Another extrapolation that can be made from data regarding sequential vs concurrent anti-endocrine therapy and RT in patients with newly diagnosed disease is that there appears to be no effect on survival with either tamoxifen or aromatase inhibitors in this case.[49,50] The one study that demonstrated a difference in these approaches was the Southwest Oncology Group (SWOG)-8814 trial, but a difference was noted only in disease-free survival and not overall survival.[51] Some preclinical evidence points to interactions between BRCA1 mutations and coactivators of ER.[52] We currently have no clinical evidence that would support a change in sensitivity to anti-endocrine treatment after chest wall radiation, and therefore the use of anti-endocrine therapy in this patient population follows the same treatment guidelines as in other newly diagnosed patients with breast cancer.
RT Following Prior Radiation for Hodgkin Lymphoma
Classically, prior chest radiation that includes breast tissue is considered a relative contraindication to subsequent breast-conserving therapy for early-stage breast cancer. A second course of radiation to the whole breast is thought to place the patient at risk for suboptimal cosmesis due to breast or skin fibrosis in areas of re-irradiation. Women in this situation have an equivalent oncologic alternative (mastectomy) without the risks associated with a second course of radiation. A few small studies, however, have challenged this standard approach. In a series of 32 women with prior chest radiation who underwent whole-breast irradiation with a median dose of 50 Gy after lumpectomy for breast cancer, none of the patients developed grade 3/4 acute radiation toxicity or soft-tissue necrosis.[53] No assessment of cosmesis was made, however. A similar report from the Institut Curie described good outcomes in 30 women undergoing breast radiation after receiving chest radiation for Hodgkin lymphoma.[54] Prone whole-breast treatment is a well-established technique that in many circumstances can minimize or even eliminate the chest wall from whole-breast treatment.
A recent Radiation Therapy Oncology Group phase II trial of repeat breast-conserving surgery and three-dimensional conformal partial breast re-irradiation for local recurrence of breast cancer is currently in follow-up after completing accrual of 65 women in 2013 (ClinicalTrials.gov identifier: NCT01082211).Acute toxicity rates were excellent; therefore, long-term results of this trial may expand treatment options for women with breast cancer diagnoses after treatment for Hodgkin lymphoma.
In the setting of a breast cancer case in which postmastectomy chest wall radiation would otherwise be indicated, careful consideration by an experienced radiation oncologist is essential in weighing the benefits of postmastectomy RT in preventing breast cancer recurrence and the risk to normal tissue. This would also include consideration of breast reconstruction if performed, prior details of initial chest radiation (dose and field/volume), and risks of lymphedema and damage to the brachial plexus. Individualized treatment approaches are appropriate.
Hodgkin lymphoma survivors have an increased risk of death that is not related to breast cancer; however, the risk of breast cancer–related mortality appears to be similar to that of the general population.[45] Hodgkin lymphoma survivors are four times more likely to develop a metachronous contralateral breast cancer (18%) as compared with age-matched controls (6%).[45]
Finally, there may be evidence that radiation-induced breast cancer increases DNA damage and mutational events compared with usual breast cancer. Further research is needed to determine whether these cancers appear different upon recurrence in regard to tumor heterogeneity or mutational load, and if genomic assessment of the tumor would be of benefit for treatment decision making, as it is in metastatic breast cancer at present.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Bhatia S, Yasui Y, Robison LL, et al. High risk of subsequent neoplasms continues with extended follow-up of childhood Hodgkin’s disease: report from the Late Effects Study Group. J Clin Oncol. 2003;21:4386-94.
2. Metayer C, Lynch CF, Clarke EA, et al. Second cancers among long-term survivors of Hodgkin’s disease diagnosed in childhood and adolescence. J Clin Oncol. 2000;18:2435-43.
3. Hancock SL, Tucker MA, Hoppe RT. Breast cancer after treatment of Hodgkin’s disease. J Natl Cancer Inst. 1993;85:25-31.
4. Ng AK, Bernardo MV, Weller E, et al. Second malignancy after Hodgkin disease treated with radiation therapy with or without chemotherapy: long-term risks and risk factors. Blood. 2002;100:1989-96.
5. Constine LS, Tarbell N, Hudson MM, et al. Subsequent malignancies in children treated for Hodgkin’s disease: associations with gender and radiation dose. Int J Radiat Oncol Biol Phys. 2008;72:24-33.
6. Taylor AJ, Winter DL, Stiller CA, et al. Risk of breast cancer in female survivors of childhood Hodgkin’s disease in Britain: a population-based study. Int J Cancer. 2007;120:384-91.
7. Kenney LB, Yasui Y, Inskip PD, et al. Breast cancer after childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Intern Med. 2004;141:590-7.
8. Henderson TO, Amsterdam A, Bhatia S, et al. Systematic review: surveillance for breast cancer in women treated with chest radiation for childhood, adolescent, or young adult cancer. Ann Intern Med. 2010;152:444-55; W144-54.
9. Travis LB, Hill DA, Dores GM, et al. Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA. 2003;290:465-75.
10. Travis LB, Hill D, Dores GM, et al. Cumulative absolute breast cancer risk for young women treated for Hodgkin lymphoma. J Natl Cancer Inst. 2005;97:1428-37.
11. De Bruin ML, Sparidans J, van’t Veer MB, et al. Breast cancer risk in female survivors of Hodgkin’s lymphoma: lower risk after smaller radiation volumes. J Clin Oncol. 2009;27:4239-46.
12. Veit-Rubin N, Rapiti E, Usel M, et al. Risk, characteristics, and prognosis of breast cancer after Hodgkin’s lymphoma. Oncologist. 2012;17:783-91.
13. Schaapveld M, Aleman BM, van Eggermond AM, et al. Second cancer risk up to 40 years after treatment for Hodgkin's lymphoma. N Engl J Med. 2015;373:2499-511.
14. Easton DF, Ford D, Bishop DT. Breast and ovarian cancer incidence in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Am J Hum Genet. 1995;56:265-71.
15. Easton DF, Steele L, Fields P, et al. Cancer risks in two large breast cancer families linked to BRCA2 on chromosome 13q12-13. Am J Hum Genet. 1997;61:120-8.
16. Ford D, Easton DF, Stratton M, et al. Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. The Breast Cancer Linkage Consortium. Am J Hum Genet. 1998;62:676-89.
17. Struewing JP, Hartge P, Wacholder S, et al. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med. 1997;336:1401-8.
18. Landier W, Bhatia S, Eshelman DA, et al. Development of risk-based guidelines for pediatric cancer survivors: the Children’s Oncology Group Long-Term Follow-Up Guidelines from the Children’s Oncology Group Late Effects Committee and Nursing Discipline. J Clin Oncol. 2004;22:4979-90.
19. Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57:75-89.
20. Ng AK, Garber JE, Diller LR, et al. Prospective study of the efficacy of breast magnetic resonance imaging and mammographic screening in survivors of Hodgkin lymphoma. J Clin Oncol. 2013;31:2282-8.
21. Freitas V, Scaranelo A, Menezes R, et al. Added cancer yield of breast magnetic resonance imaging screening in women with a prior history of chest radiation therapy. Cancer. 2013;119:495-503.
22. National Comprehensive Cancer Network Guidelines. Hodgkin lymphoma (version 3.2016). https://www.nccn.org/professionals/physician_gls/pdf/hodgkins.pdf. Accessed October 25, 2016.
23. Mulder RL, Kremer LC, Hudson MM, et al. Recommendations for breast cancer surveillance for female survivors of childhood, adolescent, and young adult cancer given chest radiation: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2013;14:e621-e629.
24. Richardson DB, Cardis E, Daniels RD, et al. Risk of cancer from occupational exposure to ionising radiation: retrospective cohort study of workers in France, the United Kingdom, and the United States (INWORKS). Br Med J. 2015;351:h5359.
25. Taylor C, Correa C, Anderson S, et al. Late side-effects of breast cancer radiotherapy: second cancer incidence and non-breast-cancer mortality among 40,000 women in 75 trials. San Antonio Breast Cancer Symposium; San Antonio, TX; Dec 8–12, 2015: Abstr S05-08.
26. Oeffinger KC, Ford JS, Moskowitz CS, et al. Breast cancer surveillance practices among women previously treated with chest radiation for a childhood cancer. JAMA. 2009;301:404-14.
27. Tamoxifen. https://www.drugs.com/pro/tamoxifen.html. Accessed October 25, 2016.
28. Cuzick J, Sestak I, Bonanni B, et al. Selective oestrogen receptor modulators in prevention of breast cancer: an updated meta-analysis of individual participant data. Lancet. 2013;381:1827-34.
29. Nelson HD, Smith ME, Griffin JC, Fu R. Use of medications to reduce risk for primary breast cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;158:604-14.
30. Visvanathan K, Hurley P, Bantug E, et al. Use of pharmacologic interventions for breast cancer risk reduction: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2013;31:2942-62.
31. Bevers TB, Ward JH, Arun BK, et al. Breast cancer risk reduction, version 2.2015. J Natl Compr Canc Netw. 2015;13:880-915.
32. Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371-88.
33. Iqbal J, Ginsburg OM, Wijeratne TD, et al. Endometrial cancer and venous thromboembolism in women under age 50 who take tamoxifen for prevention of breast cancer: a systematic review. Cancer Treat Rev. 2012;38:318-28.
34. Cuzick J, Sestak I, Cawthorn S, et al. Tamoxifen for prevention of breast cancer: extended long-term follow-up of the IBIS-I breast cancer prevention trial. Lancet Oncol. 2015;16:67-75.
35. Powles TJ, Ashley S, Tidy A, et al. Twenty-year follow-up of the Royal Marsden randomized, double-blinded tamoxifen breast cancer prevention trial. J Natl Cancer Inst. 2007;99:283-90.
36. Veronesi U, Maisonneuve P, Rotmensz N, et al. Tamoxifen for the prevention of breast cancer: late results of the Italian Randomized Tamoxifen Prevention Trial among women with hysterectomy. J Natl Cancer Inst. 2007;99:727-37.
37. Pruthi S, Heisey RE, Bevers TB. Chemoprevention for breast cancer. Ann Surg Oncol. 2015;22:3230-5.
38. Roetzheim RG, Lee JH, Fulp W, et al. Acceptance and adherence to chemoprevention among women at increased risk of breast cancer. Breast. 2015;24:51-6.
39. Bambhroliya A, Chavez-MacGregor M, Brewster AM. Barriers to the use of breast cancer risk reduction therapies. J Natl Compr Canc Netw. 2015;13:927-35.
40. Burke EE, Portschy PR, Tuttle TM. Prophylactic mastectomy: who needs it, when and why. J Surg Oncol. 2015;111:91-5.
41. De Bruin ML, Sparidans J, van't Veer MB, et al. Breast cancer risk in female survivors of Hodgkin’s lymphoma: lower risk after smaller radiation volumes. J Clin Oncol. 2009;27:4239-46.
42. Fermé C, Eghbali H, Meerwaldt JH, et al. Chemotherapy plus involved-field radiation in early-stage Hodgkin's disease. N Engl J Med. 2007;357:1916-27.
43. Engert A, Plütschow A, Eich HT, et al. Reduced treatment intensity in patients with early-stage Hodgkin's lymphoma. N Engl J Med. 2010;363:640-52.
44. Yahalom J, Illidge T, Specht L, et al. Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys. 2015;92:11-31.
45. Elkin EB, Klem ML, Gonzales AM, et al. Characteristics and outcomes of breast cancer in women with and without a history of radiation for Hodgkin’s lymphoma: a multi-institutional, matched cohort study. J Clin Oncol. 2011;29:2466-73.
46. American Cancer Society. Breast cancer facts & figures, 2015-2016. http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-046381.pdf. Accessed October 25, 2016.
47. De Bruin ML, Sparidans J, van't Veer MB, et al. Breast cancer risk in female survivors of Hodgkin's lymphoma: lower risk after smaller radiation volumes. J Clin Oncol. 2009;27:4239-46.
48. Kauff ND, Domchek SM, Friebel TM, et al. Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: a multicenter, prospective study. J Clin Oncol. 2008;26:1331-7.
49. Ahn PH, Vu HT, Lannin D, et al. Sequence of radiotherapy with tamoxifen in conservatively managed breast cancer does not affect local relapse rates. J Clin Oncol. 2005;23:17-23.
50. Valakh V, Trombetta MG, Werts ED, et al. Influence of concurrent anastrozole on acute and late side effects of whole breast radiotherapy. Am J Clin Oncol. 2011;34:245-8.
51. Albain KS, Barlow WE, Ravdin PM, et al. Adjuvant chemotherapy and timing of tamoxifen in postmenopausal patients with endocrine-responsive, node-positive breast cancer: a phase 3, open-label, randomised controlled trial. Lancet. 2009;374:2055-63.
52. Wen J, Li R, Lu Y, Shupnik MA. Decreased BRCA1 confers tamoxifen resistance in breast cancer cells by altering estrogen receptor-coregulator interactions. Oncogene. 2009;28:575-86.
53. Terenziani M, Massimino M, Magazzù D, et al. Management of breast cancer after Hodgkin's lymphoma and paediatric cancer. Eur J Cancer. 2015;51:1667-74.
54. Haberer S, Belin L, Le Scodan R, et al. Locoregional treatment for breast carcinoma after Hodgkin's lymphoma: the breast conservation option. Int J Radiat Oncol Biol Phys. 2012;82:e145-e152.