Breast Cryoablation Inhibits Recurrence, Enhances Survival in Breast Cancer
Findings from the ICE3 trial revealed that no serious adverse effects were experienced related to the use of cryoablation in ipsilateral breast tumors.
Findings from the ICE3 trial revealed that no serious adverse effects were experienced related to the use of cryoablation in ipsilateral breast tumors.
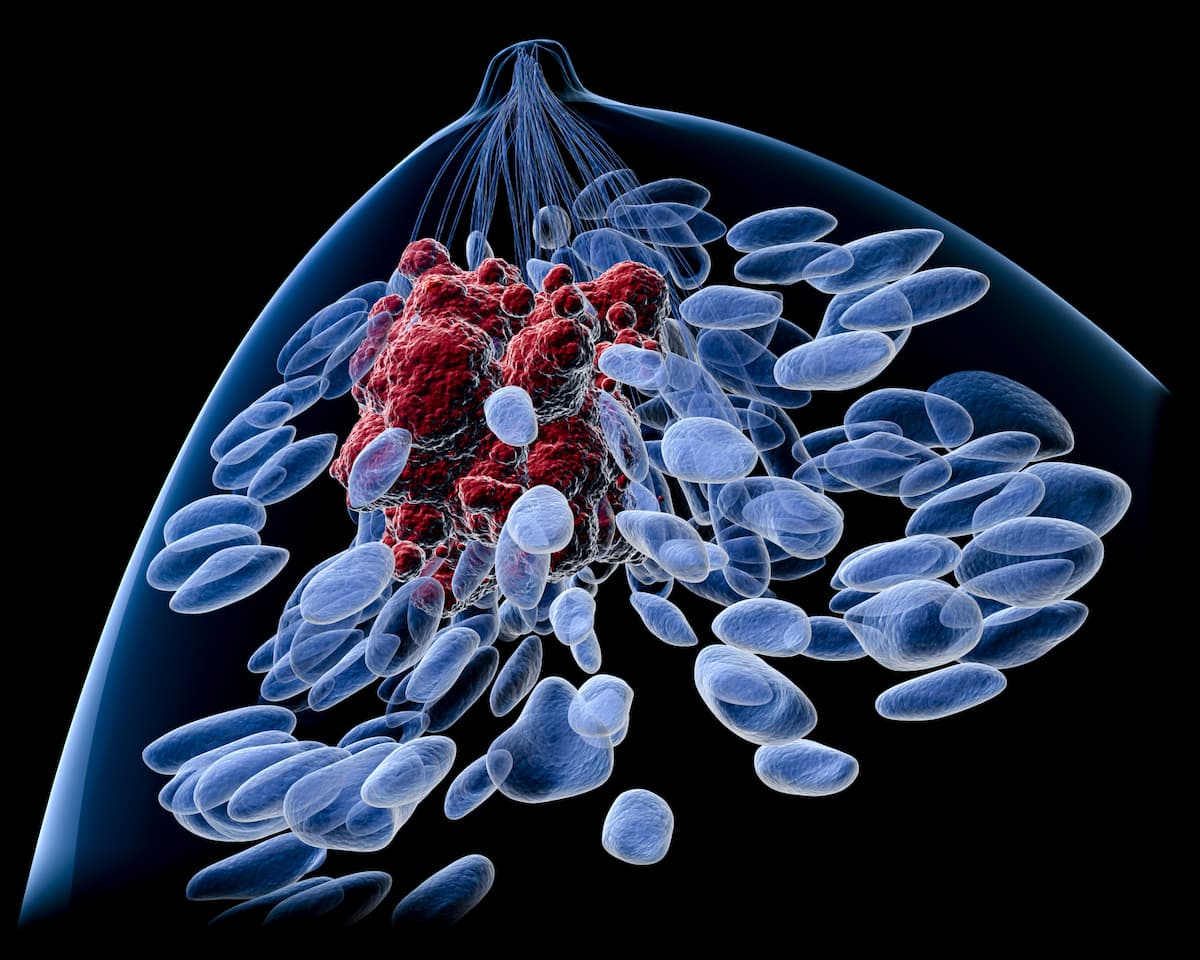
Breast cryoablation elicited low recurrence and high survival rates in women 60 years or older with low-risk, early-stage breast cancers, offering a promising alternative to surgery for this patient population, according to findings from the ICE3 trial (NCT02200705) published in the Annals of Surgical Oncology.1
Data from the trial showed at a median follow-up of 54.16 ± 13.07 months, the overall ipsilateral breast tumor recurrence (IBTR) rate was 3.61% among patients successfully treated with cryoablation eligible for follow-up. Additionally, the IBTR rate at 60, 48, and 36 months were 4.3% (95% CI, 2.1%-8.7%), 1.7% (95% CI, 0.6%-5.3%), and 0.6% (95% CI, 0.1%-3.9%), respectively, based on Kaplan-Meier estimate.
Seven ipsilateral recurrence cases were reported on study, in addition to 2 cases of distant metastases and 4 cases of second primary breast cancer, with a 5-year disease-free survival (DFS) rate of 92.8% (95% CI, 87.6%-95.8%).The breast cancer survival rate was 96.7% (95% CI, 92.2%-98.6%) in patients treated with cryoablation, with 2 patient deaths due to distant metastases and 3 due to unknown reasons. Furthermore, the overall survival (OS) rate was 88.6% (95% CI, 82.9%-92.5%).
“Our 5-year analysis of the trial’s primary outcome, IBTR at 5 years, suggests that cryoablation is safe and effective for patients with low-risk, early-stage breast cancer,” Richard E. Fine, MD, FACS, breast surgeon at the Margaret West Comprehensive Breast Center, wrote in the publication with study coinvestigators.1 “During the 5-year follow-up period, IBTR in our low-risk breast cancer cohort showed local control similar to that with surgical standard of care while avoiding the potential risks of a surgical procedure. Cryoablation may be considered as an alternative to lumpectomy in this select population if followed by appropriate adjuvant treatment.”
The Institutional Review Board (IRB)-approved ICE3 trial enrolled and treated 194 female patients at least 60 years of age with unifocal, ultrasound-visible invasive ductal carcinoma 1.5 cm or smaller in size and with a low-risk cancer profile. Cryoablation was performed with the ProSense Cryosurgical System, which utilized liquid nitrogen to freeze target lesions.
Treatment consisted of a double freezing method, wherein patients received cryoablation for a minimum of 9 mins, a passive thaw for 8 mins, and a second 9-min freeze. Treatment times were controlled at the discretion of the investigator, with adjustments made to achieve at least 35-mm ice ball at the end of the first freeze and a 40-mm ice ball at the end of the second freeze, at a maximum of 12 minutes.
Patients on study had a median age of 74.5 years (range, 55-94). Most patients were Caucasian (82.5%), all patients had estrogen receptor (ER)–positive or HER–negative receptor status, 92.8% had PR-positive receptor status, and 51% had a Nottingham tumor score of intermediate. The median tumor size by ultrasound was 8.1 mm (range, 2.5-14.9) for the sagittal dimension, 7.4 mm (range, 2.8-14) for the transverse dimension, and 6.3 mm (range, 1-14) for anterior-posterior dimension.
The primary study end point was IBTR at 5 years. Secondary end points included DFS, quality of life, breast cancer survival, OS, and safety.2
In total, 97 patients reported 187 device-related non-serious adverse effects (AEs). Most AEs reported were mild in severity (88.2%, Common Terminology Criteria for Adverse Events [CTCAE] grade 1), with moderate (CTCAE grade 2) and severe AEs (CTCAE grade 3) occurring in 9.6% and 2.1% of patients, respectively. The most common mild AEs included bruising (25.7%), pain in needle insertion (20.9%), and localized edema (19.3%).
Additionally, the most common moderate AEs included bruising (5.3%), edema (1.6%), skin burns (1.1%), and pain (1.1%), and the only reported severe AE was bruising in 2.1% of patients. All AEs were resolved without residual effects, and 16 patients died due to reasons unrelated to breast cancer while on study.
References
- Fine RE, Gilmore RC, Tomkovich KR, et al. Cryoablation without excision for early-stage breast cancer: ICE3 trial 5-year follow-up on ipsilateral breast tumor recurrence. Ann Surg Oncol. 2024;31:7273-7283. doi:10.1245/s10434-024-16181-0
- Cryoablation of low risk small breast cancer- ICE3 trial. ClinicalTrials.gov. Updated May 29, 2024. Accessed February 4, 2025. https://tinyurl.com/4na8254s