Brentuximab Vedotin Combination Improves Survival in Pretreated R/R DLBCL
Brentuximab vedotin, lenalidomide, and rituximab yielded a median OS of 13.8 months and a median PFS of 4.2 months in the phase 3 ECHELON-3 trial.
Brentuximab vedotin, lenalidomide, and rituximab yielded a median OS of 13.8 months and a median PFS of 4.2 months in the phase 3 ECHELON-3 trial.
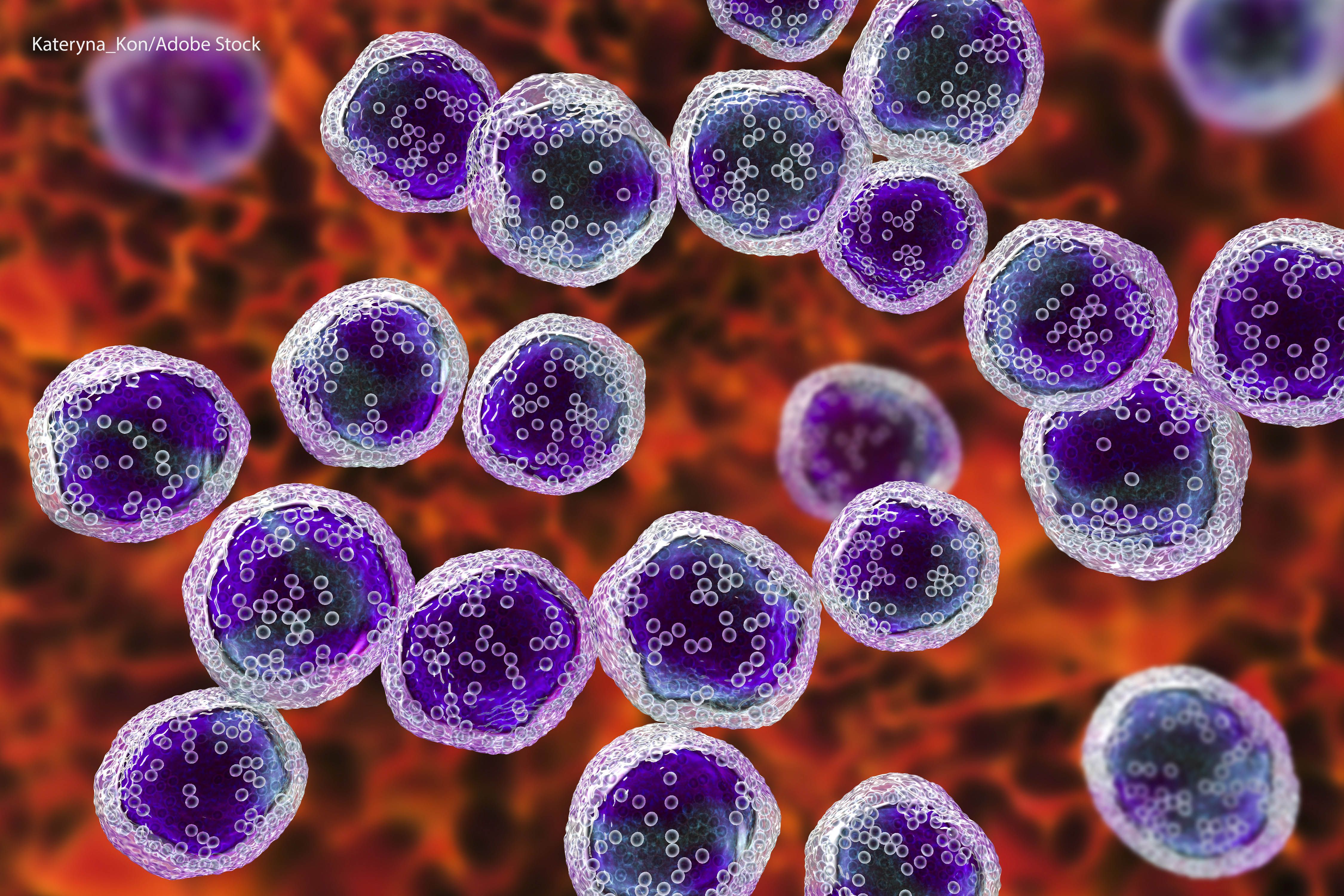
Brentuximab vedotin (Adcetris) with lenalidomide (Revlimid) and rituximab (Rituxan) elicited a statistically significant survival benefit and acceptable safety profile compared with placebo plus lenalidomide and rituximab in heavily pretreated patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL), according to data from the randomized, double-blind phase 3 ECHELON-3 trial (NCT04404283) published in the Journal of Clinical Oncology.
At a median follow-up of 16.4 months, the median overall survival (OS) in the experimental arm—in which patients received brentuximab vedotin with lenalidomide and rituximab—was 13.8 months (95% CI, 10.3-18.8) vs 8.5 months (95% CI, 5.4-11.7) with placebo plus lenalidomide and rituximab in the control arm (HR, 0.63; 95% CI, 0.45-0.89; P = .009). The median progression-free survival (PFS) was 4.2 months (95% CI, 2.9-7.1) in the experimental arm and 2.6 months (95% CI, 1.4-3.1) in the control arm (HR, 0.53; 95% CI, 0.38-0.73; P <.001).
The overall response rate (ORR) was 64% (95% CI, 55%-73%; P <.001) in the experimental arm and 42% (95% CI, 33%-51%) in the control arm. Complete response (CR) rates were 40% in the experimental arm and 19% in the control arm; the median duration of CR was 18.9 months (95% CI, 11.1-not evaluable [NE]) and NE (95% CI, 2.8-NE). The median duration of response (DOR) was 8.3 months (95% CI, 4.2-15.3) in the experimental group and 3.0 months (95% CI, 2.8-5.4) in the control group.
“ECHELON-3 is the first randomized controlled study to demonstrate survival benefit in patients with [relapsed/refractory] DLBCL in the third-line or later setting; efficacy was observed across high-risk subgroups,” lead study author Nancy L. Bartlett, MD, Koman Professor of Medical Oncology in the Division of Oncology at Washington University School of Medicine in St. Louis, and coauthors, wrote in the journal. “ECHELON-3 could potentially affect the treatment landscape for [relapsed/refractory] DLBCL by supporting the use of [brentuximab vedotin plus lenalidomide and rituximab] in this patient population.”
A total of 230 patients were randomly assigned, in a 1:1 ratio, and stratified by CD30 expression (positive vs negative), cell of origin (germinal center B vs non-germinal center B cell), previous treatment with CAR T-cell therapy (received or not), and previous hematopoietic stem-cell transplant therapy (received or not), to either the experimental arm (n = 112) or the control arm (n = 118).
Patients received 1.2 mg/kg of brentuximab vedotin or placebo intravenously once every 3 weeks, 20 mg of oral lenalidomide once daily, and 375 mg/m2 of rituximab intravenously once every 3 weeks in 21-day cycles. From cycle 2 onward, 1400 mg of subcutaneous rituximab was permitted.
Eligible patients were 18 years or older with relapsed/refractory DLBCL who received at least 2 prior lines of systemic therapy. They also had to be ineligible for hematopoietic stem-cell transplant or CAR T-cell therapy and have an ECOG performance status from 0 to 2.
The most common previous systemic therapies received were anthracycline (98% in the experimental arm and 97% in the control arm), an anti-CD20 antibody (98% and 97%, respectively), CAR T-cell therapy (29% and 30%), a bispecific antibody (13% and 17%), and autologous stem-cell transplant (9% and 15%). The majority of patients had disease refractory to their last previous DLBCL therapy (88% and 81%, respectively).
The trial’s primary end point was OS. Key secondary end points were PFS, ORR, CR rate, duration of response per Lugano classification, adverse events (AEs), and OS in the CD30-positive subgroup.
Regarding safety, treatment-emergent AEs (TEAEs) of any grade occurred in 97% of patients in the experimental group and 97% of patients in the control group; TEAEs of grade 3 or higher occurred in 88% and 77%, respectively. The most common TEAEs of grade 3 or higher were neutropenia (43% vs 28%), thrombocytopenia (25% vs 19%), anemia (22% vs 21%), and pneumonia (11% vs 5%).
Serious TEAEs occurred in 60% of patients in the experimental arm and 50% of patients in the control arm; the most common were pneumonia (11% vs 5%), COVID-19 (7% vs 5%), COVID-19 pneumonia (7% vs 3%), and febrile neutropenia (6% vs 5%).
TEAEs led to dose modifications in 76% of patients in the experimental arm and 48% of patients in the control arm; treatment discontinuation occurred in 15% and 9%, respectively. TEAEs associated with deaths occurred in 12% and 8%, mainly due to COVID-19–related events.
Reference
Bartlett NL, Hahn U, Kim W-S, et al. Brentuximab vedotin combination for relapsed diffuse large B-cell lymphoma. J Clin Oncol. Published online January 7, 2025. doi:10.1200/JCO-24-02242
Highlighting Insights From the Marginal Zone Lymphoma Workshop
Clinicians outline the significance of the MZL Workshop, where a gathering of international experts in the field discussed updates in the disease state.