Camizestrant Significantly Improves PFS in HER2– Breast Cancer
Camizestrant showed better progression-free survival than fulvestrant across various subgroups of patients with advanced breast cancer.
Camizestrant showed better progression-free survival than fulvestrant across various subgroups of patients with advanced breast cancer.
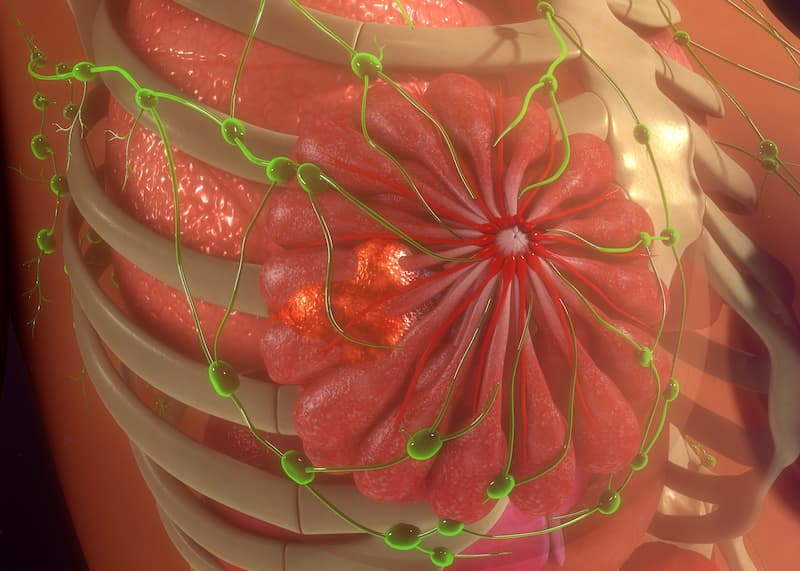
Patients with estrogen receptor–positive, HER2-negative, advanced breast cancer experienced improved progression-free survival (PFS) on camizestrant vs fulvestrant (Faslodex), findings from the open-label, randomized phase 2 SERENA-2 trial (NCT04214288) showed.
Patients were randomly assigned into groups where they were either assigned 75 mg doses of camizestrant, 150 mg doses of camizestrant, 300 mg doses of camizestrant, or 500 mg doses of fulvestrant.
The median PFS in the camizestrant 75 mg group was 7.2 months (90% CI, 3.7-10.9), 7.7 months (90% CI, 5.5-12.9) in the camizestrant 150 mg group, and 3.7 months (90% CI, 2.0-6.0) with fulvestrant. Median follow-up was 16.6 months (IQR, 12.9-19.4) for the 75 mg camizestrant group, 16.3 months (IQR, 12.9-18.3) for the 150 mg camizestrant group, and 14.7 months (IQR, 12.7-20.1) for the fulvestrant group.
For the 75 mg dose of camizestrant group, the hazard ratio vs fulvestrant was 0.59 (90% CI, 0.42-0.81, P=.017). For the 150 mg dose of camizestrant group, the hazard ratio vs fulvestrant was 0.64 (90% CI, 0.46 to 0.89, P=.009).
“In SERENA-2, treatment with camizestrant at daily doses of 75 mg and 150 mg produced a significant improvement in investigator-assessed PFS compared with fulvestrant at a monthly dose of 500 mg in patients with estrogen receptor-positive, HER2-negative advanced breast cancer who had progressed on endocrine therapy,” the authors of the study wrote.
A total of 240 patients were enrolled and randomly assigned to either orally administered, once daily 75 mg doses of camizestrant (n = 74), 150 mg of camizestrant (n = 73), or 300 mg of camizestrant (n= 20); or intramuscular injections of 500 mg of fulvestrant (n = 73) given on days 1, 15, and 29, then in 4-week cycles until disease progression. The median age was 60 years (IQR, 54-69), and 226 of 240 patients (94%) were white.
Patients had to be female, 18 years or older, and postmenopausal with cytologically or histologically confirmed metastatic or locoregionally recurrent adenocarcinoma of the breast and documented estrogen receptor–positive and HER2-negative status. Eligibility required objective evidence of progression on or after the last systemic therapy and measurable disease according to RECIST criteria and an ECOG performance status of 0 or 1 with at least 12 weeks of life expectancy and no deterioration over the past 2 weeks.
The primary end point was investigator-assessed PFS. Secondary end points included objective response rate, clinical benefit rate, and overall survival (OS).
At the data cutoff of the primary analysis, investigator-assessed PFS events were recorded in 50 of 74 (68%) patients in the 75 mg camizestrant group, 48 of 73 (66%) patients in the 150 mg camizestrant group, and 57 of 73 (78%) patients in the fulvestrant group.
Overall, 11 (16%) of 70 patients in the 75 mg camizestrant group, 11 (17%) of 65 patients in the 150 mg camizestrant group, and 8 (12%) of 68 patients in the fulvestrant group had an objective response. Patients in the 75 mg camizestrant group (47%) and the 150 mg group (49%) showed higher rates of clinical benefit at 25 weeks compared with the fulvestrant group (38%).
Data on OS were 26% mature for the primary analysis. At data cutoff, 23 of 74 patients (31%) in the camizestrant 75 mg group, 14 of 73 (19%) in the camizestrant 150 mg group, and 21 of 73 (29%) in the fulvestrant group had died. The median OS in the fulvestrant group was 20.5 months (90% CI, 19.6 to not calculated).
Treatment-related adverse events (AEs) happened to 39 of 74 (53%) patients in the 75 mg camizestrant group, 49 of 73 (67%) patients in the 150 mg camizestrant group, 14 of 20 (70%) patients in the 300 mg camizestrant group, and 13 of 73 (18%) of patients in the fulvestrant group.
In 9 of 72 (12%) patients in the camizestrant 75 mg group, 18 of 73 (25%) patients in the camizestrant 150 mg group, and 7 of 20 (35%) patients in the camizestrant 300 mg group, photopsia occurred. It did not occur to any patients in the fulvestrant group. No doses were interrupted, and no patient discontinued treatment because of photopsia.
Of grade 3 or worse treatment-emergent AEs, none occurred in 2 or more patients in the camizestrant 75 mg group, fatigue (n = 2) and hypertension (n= 2) occurred in the camizestrant 150 mg group, none occurred in the camizestrant 300 mg group, and anemia (n = 2) and pleural effusion (n = 2) occurred in the fulvestrant group.
There was 1 treatment-emergent death in the camizestrant 150 mg group due to COVID-19 pneumonia. No treatment-related deaths were reported.
Reference
Oliveira M, Pominchuk D, Nowecki Z, et al. Camizestrant, a next-generation oral SERD, versus fulvestrant in post-menopausal women with oestrogen receptor-positive, HER2-negative advanced breast cancer (SERENA-2): a multi-dose, open-label, randomised, phase 2 trial. Lancet Oncol. 2024;25(11):1424-1439. doi:10.1016/S1470-2045(24)00387-5