Cediranib Delays Disease Progression in Advanced Cervical Cancer
Adding the TKI cediranib to chemotherapy improved progression-free survival in patients with metastatic or relapsed cervical cancer, according to a study presented at the 2014 ESMO Congress.
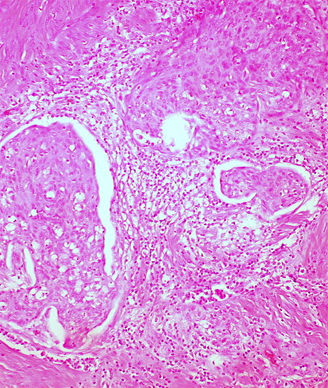
Invasive squamous carcinoma of the cervix, cold knife cone; source: Ed Uthman, Wikimedia Commons
Adding the tyrosine kinase inhibitor (TKI) cediranib to chemotherapy improved progression-free survival (PFS) in patients with metastatic or relapsed cervical cancer, according to a new phase II study.
“Cervical cancers with a well-developed blood supply can have a particularly bad outcome,” said Paul Symonds, MD, of the University Leicester in the United Kingdom, in a press release. “The experimental drug cediranib blocks the cell surface receptor VEGF, which stimulates the growth of new blood vessels to feed the growth of tumors.”
Generally, patients with metastatic or recurrent cervical cancers do not fare well with standard chemotherapy, with only about 20% to 30% response rates. In the new study, researchers randomized 69 patients to either carboplatin, paclitaxel, and cediranib 20 mg daily (34 patients), or carboplatin, paclitaxel, and placebo (35 patients). Results were presented at the European Society for Medical Oncology (ESMO) 2014 Congress in Madrid.
Of the full cohort, 83% had one previous line of treatment, and 79% completed at least 6 cycles of chemotherapy; 22% of placebo patients and 17% of cediranib patients stopped therapy due to treatment-related reasons.
The median PFS was 30 weeks for the placebo patients and 35 weeks for the cediranib patients, for a hazard ratio (HR) for progression of 0.61 (80% CI, 0.41-0.89; P = .046). The median change in VEGF inhibition was also significantly improved with cediranib.
The median overall survival was not different between the groups, at 63 weeks for placebo and 59 weeks for cediranib (P = .401). The overall response rate was 42% for placebo and 59% for the study drug (P = .030). There was some increase in toxicity with cediranib; 50% of patients experienced grades 2/3/4 diarrhea, compared with only 18% in the placebo group (P = .005). Hypertension was also increased with cediranib. Overall, 9% of placebo patients and 19% of cediranib patients experienced a grade 2 or higher toxicity, but the authors said these toxicities were manageable.
“Recurrent or metastatic cervical cancer is really difficult to treat with a low response rate and poor survival,” Symonds said. “This study has opened up a new avenue of investigation for a difficult-to-treat cancer.”
Andres Poveda, MD, of the Fundación Instituto Valenciano de OncologÃa in Valencia, Spain, was the discussant for this study, and noted that angiogenesis inhibition does seem to be a very promising approach to recurrent cervical cancer. The US Food and Drug Administration approved the angiogenesis inhibitor bevacizumab for persistent, recurrent, or metastatic cervical cancer in August of this year. “We are now waiting for phase III results to confirm the favorable predictions of this treatment with cediranib,” Poveda said.