Cetuximab-Associated Infusion Reactions: Pathology and Management
Cetuximab (Erbitux), a chimeric antiepidermal growth factor receptor monoclonal antibody currently used to treat metastatic colorectal cancer, is in clinical development for several other solid tumors. Although cutaneous manifestations are the most common toxicities associated with cetuximab, they are rarely life-threatening. Cetuximab-related infusion reactions are less common, but they may become severe and cause fatal outcomes if not managed appropriately. Little about the specific etiology of these events is known; however, an overview of infusion reactions observed with other compounds may shed some light and help characterize cetuximab-related reactions. For physicians administering cetuximab, familiarity with acute reaction treatment protocols and preparedness to identify and manage symptoms promptly and effectively are most important to minimize potential risks.
Cetuximab (Erbitux), a chimeric antiepidermal growth factor receptor monoclonal antibody currently used to treat metastatic colorectal cancer, is in clinical development for several other solid tumors. Although cutaneous manifestations are the most common toxicities associated with cetuximab, they are rarely life-threatening. Cetuximab-related infusion reactions are less common, but they may become severe and cause fatal outcomes if not managed appropriately. Little about the specific etiology of these events is known; however, an overview of infusion reactions observed with other compounds may shed some light and help characterize cetuximab-related reactions. For physicians administering cetuximab, familiarity with acute reaction treatment protocols and preparedness to identify and manage symptoms promptly and effectively are most important to minimize potential risks.
The epidermal growth factor receptor (EGFR) is an important therapeutic target in treating cancer. Overexpression of EGFR, an indicator of poor prognosis,[1,2] occurs in several malignancies, including colorectal, pancreatic, and head and neck cancers, as well as non-small-cell lung cancer (NSCLC).[3,4] Recently, agents that include small-molecule tyrosine kinase inhibitors and monoclonal antibodies have been developed that target EGFR. Randomized trials with cetuximab (Erbitux), a chimeric anti-EGFR monoclonal antibody composed of the variable regions of a murine anti-EGFR antibody with human immunoglobulin (Ig) G1 constant regions, have demonstrated important antitumor activity in metastatic colorectal cancer and head and neck cancer.
In irinotecan (Camptosar)-refractory metastatic colorectal cancer, disease control (defined as response or stable disease) was achieved in 32% of patients on cetuximab monotherapy and 56% of those given a combination of cetuximab and irinotecan.[5] In head and neck cancer, cetuximab therapy plus radiation prolonged survival when compared with radiotherapy alone (median survival: 54 vs 28 months; P = .02).[6]
Although its overall safety profile is favorable, cetuximab therapy has been complicated by acute infusion-related reactions. This review will describe the types of acute infusion-related reactions reported with cetuximab, compare them with infusion-related reactions seen with other antineoplastic agents, and suggest recommendations for managing these reactions in the clinic.
Cetuximab Safety Overview
TABLE 1

Adverse Events in Advanced Colorectal Cancer Patients Receiving Cetuximab
The overall safety profile of cetuximab is favorable; however, adverse events (Table 1) have been reported in clinical trials of cetuximab given alone for advanced colorectal cancer.[7] The majority of toxicities were of grade 1 or 2 severity, as defined by the Cancer Therapy Evaluation Program Common Toxicity Criteria for Adverse Events (CTEP-CTCAE), version 2.0. Current criteria for evaluating these toxicities are presented in Table 2.[8]
The most common toxicity related to cetuximab therapy is an acneiform rash noted among 72% to 90% of all advanced colorectal cancer patients treated with cetuximab in clinical trials. The majority of these rashes were mild or moderate in nature, although 6% to 18% of patients developed a grade 3 or 4 rash.[5,9-12] This dermatologic manifestation probably results from inhibition of EGFR in the skin; the histology of rash lesions usually involves neutrophilic infiltration in dermal tissues (particularly in the infundibular region of the hair follicle) and loss of differentiation in the stratumcorneum of the epidermis, without presence of comedones. This unique histology indicates this rash is a pathologic entity different from acne or hypersensitivity-related manifestations.[13]
TABLE 2

Grading of Most Relevant Cetuximab-Related Toxicities
Infusion reactions of all severities occurred in approximately 20% of colorectal cancer patients participating in trials using cetuximab alone or with irinotecan. Approximately 3% of patients developed severe reactions (grade 3 or 4), and a small number of these events (< 0.1% of all patients) were fatal.[5,7,9-12]
Preliminary reports of randomized trials with cetuximab in advanced head and neck cancer and NSCLC indicate that the safety profile of cetuximab is very similar in these settings; further, the monoclonal antibody has not worsened toxicity associated with conventional cytotoxic or radiation therapies. Among these trials, grade 3/4 reactions described as infusion reactions or hypersensitivity reactions occurred in 2% to 7% of patients.[6,14,15]
Reactions to Monoclonal Antibodies
FIGURE 1
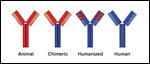
Monoclonal Antibodies
Monoclonal antibodies can be divided into four categories based on the origin of their different domains: animal, chimeric, humanized, or human (Figure 1).[16]
Monoclonal antibodies derived from animal sources, most commonly mice,[17] elicit the formation of human antimouse antibodies (HAMAs) and are substantially immunogenic, which limits multiple dosing schedules of these agents.[18-20] Subsequent investigations have focused on engineering antibodies to limit or eliminate the murine portions in the molecule. Three general methods currently are used to achieve this goal: (1) combining the full murine variable region of an antibody with the human constant region to create a chimeric antibody, (2) adding only the complementarity-determining regions (or hypervariable regions) of the murine variable regions to a human IgG framework to create a humanized antibody, and (3) using phage-display technology to screen for human-derived hypervariable regions to create a fully human monoclonal antibody.[21-24] The formation of HAMAs is reduced with these newer molecules-HAMAs developed in approximately 75% of patients during early trials of murine monoclonal antibodies,[18-20] whereas reported rates of HAMA development using modern molecules fell below 15%.[7,25,26]
Although these newer therapeutic monoclonal antibodies feature lower immunogenicity, they can still induce various types of acute infusion-related reactions with unclear underlying mechanisms.[5,27-29] Many of these reactions are mild-to-moderate in severity; however, severe reactions occur with an incidence of < 5%, generally.[7,30,31] Rarely, patients have died from these reactions.[7,27,31]
Infusion Reactions: Clinical Experience Across Therapeutic Agents
Infusion reactions occur with a wide variety of therapeutic agents, including cytotoxic agents and biologic agents such as monoclonal antibodies.[27,32-34] The characteristics of these reactions vary in symptoms, time course, and severity. A small, yet significant, percentage of patients experience acute, severe, infusion-related, potentially life-threatening adverse reactions.
As physicians integrate cetuximab into their cancer treatment strategies, they must become familiar with the identification and management of cetuximab-associated reactions. We will review clinical experience involving similar agents. Observations related to agents that have been available longer than cetuximab contribute to our current understanding of the potential mechanisms behind these reactions and may help us to manage cetuximab-related infusion reactions more effectively.
Severe Reactions
Depending on their underlying immunologic basis, severe infusion-related reactions may be categorized as either anaphylactic or anaphylactoid in nature. Fundamentally, anaphyl-actic reactions are IgE-mediated, whereas anaphylactoid reactions are not.[35]
Anaphylactic reactions are caused by rapid release of immune mediators from tissue mast cells and peripheral blood basophils triggered by IgE. Anaphylactoid reactions, also referred to as pseudoallergic reactions, mimic the symptoms of anaphylactic reactions.[35] They are caused by the direct release of mediators from mast cells and basophils in the absence of specific IgE antibodies or antigen-antibody bridging on the mast or basophil cell membrane.[35]
Clinically, "anaphylaxis" typically describes a rapid systemic reaction that involves a constellation of symptoms including wheezing/bronchospasm, angioedema (particularly laryngeal edema), hypotension, pruritus, urticaria, gastrointestinal sequelae (nausea, vomiting, pain, diarrhea), uterine contractions, and/or direct cardiac effects such as arrhythmias. Symptoms typically appear within moments of exposure, although, less commonly, the reaction may be delayed for 30 to 60 minutes or longer. Because these symptoms have a rapid onset and life-threatening potential, the clinician must be familiar with them and their time course to identify severe cases as quickly as possible.
Other Agents
Careful examination of the similarities and differences between reactions associated with other agents may yield valuable insights on the etiology and management of cetuximab-related reactions. Perhaps the best known type of reaction occurs with the use of paclitaxel,[32,36] a small-molecule taxane that blocks cell division by inhibiting tubulin depolymerization and that currently is used across tumor types, from those involving the breast to NSCLC.[32] Paclitaxel reactions may be caused by either direct mast cell degranulation by the drug's excipient, Cremophor EL (a polyethoxylated castor oil)[37] or the involvement of sensory neuropeptides.[38] These reactions differ from those observed with monoclonal antibodies in time course and symptomatology.
The most data on infusion reactions exists for the monoclonal antibody trastuzumab (Herceptin).[27] Trastuzumab inhibits HER2, a growth factor receptor from the same family as EGFR, and currently is used against HER2-overexpressing breast tumors.
TABLE 3

Characteristics of Infusion-Related Reactions With Three Antitumor Agents of Different Classes
Table 3 compares the characteristic infusion-related reactions associated with each of these compound classes.[25,27,32,33,39-42] Key timing features distinguish the onset of these reactions. Trastuzumab reactions typically are associated with the first infusion and generally occur within the first 2 hours after administration. Paclitaxel-related reactions also tend to occur shortly (10 minutes) after administration of the first infusion.[27,39,40] Reactions to oxaliplatin (Eloxatin), however, usually do not appear at first infusion; instead, they occur after repeated administration.[27,41]
Some characteristics of acute infusion-related reactions associated with monoclonal antibodies suggest that they may not be IgE-mediated. First, these reactions typically occur with the first infusion; the lack of prior sensitization argues against development of specific IgE antibodies against these agents.[27,43] Second, rechallenges have resulted in repeated reactions in few patients.[27,43] In retrospective studies of trastuzumab, 39 patients who suffered serious infusion reactions were rechallenged, and 33 (85%) of these successfully continued therapy.[27] Further, in a single-center report using infliximab (Remicade), an antitumor necrosis factor chimeric antibody, 21 patients who experienced mild or moderate infusion-related reactions were able to receive further therapy if given prophylactic medications.[43] Of three patients who were retreated following severe reactions, two had no further reactions, and one had a repeated severe acute reaction. Third, the lack of IgE-mediated anaphylaxis was further corroborated by findings that serum tryptase levels were normal in 11 patients who experienced 14 acute infusion reactions after receiving infliximab.[43]
Different mechanisms may occur in different patients; severe reactions may be anaphylactic, whereas less severe reactions would be anaphylactoid. Data concerning infusion reactions linked to radiographic contrast material suggested this variable etiology-a retrospective study found that specific IgE is present in < 4% of patients who have reactions.[44] However, in a separate study, specific IgE was found in all patients suffering severe reactions, and histamine and tryptase release correlated with the severity of the reaction.[44]
Cetuximab-Associated Infusion Reactions
Clinical trials testing cetuximab used alone or with irinotecan in advanced colorectal cancer provide the most complete characterization of infusion-related reactions associated with the monoclonal antibody. Grade 1 or 2 infusion reactions occurred in 16% of patients receiving cetuximab plus irinotecan and in 19% of those receiving cetuximab alone[7]; these included chills, fever, and dyspnea.[8] The incidence of grade 3 or 4 reactions associated with cetuximab in clinical trials ranged from 2.3% to 5%.[5,9,10]
Severe reactions typically were characterized by rapid onset of airway obstruction (bronchospasm, stridor, hoarseness), urticaria, and/or hypotension.[8] Approximately 90% of severe reactions were associated with the first infusion; however, some were associated with later infusions.[7] These reactions occurred despite use of prophylactic antihistamines and were not reliably predicted by the use of a test dose (20 mg of cetuximab was administered IV over 10 minutes prior to the initial loading dose in all patients enrolled in clinical trials).[7] Fatalities, although rare (occurring in < 0.1% of patients), did occur.[7]
Other limited data are available from clinical studies of cetuximab in various tumor types and a cetuximab safety review.[5,9,10,14,15,45-47] In these reports, infusion reactions were generally described as being hypersensitivity, allergic, anaphylactic, or anaphylactoid reactions that were characterized by such clinical symptoms as shortness of breath and chest tightness.[45]
A few trials have provided information on the time course, management, and/or outcome of patients experiencing these reactions. The safety review reported that allergic reactions occurred in 31 of 419 patients (7.4%) treated with cetuximab.[46] Of these reactions, 11 (2.6%) were of grade 3 severity and 6 (1.4%) were of grade 4 severity and were described as being anaphylactic reactions. The majority of all reactions occurred with the first dose, but 8 of the 25 patients (33%) who developed grade ≥ 3 reactions did so with later infusions. Conversely, all of the grade 4 reactions occurred within minutes of the first infusion.[46]
The true etiology of cetuximab infusion-related reactions remains unclear. As with reports of such reactions related to the use of other monoclonal antibodies, the fact that the majority of reactions occur with the first dose would suggest that these reactions are not IgE-mediated. One possible explanation for this discrepancy is that patients who develop reactions may have been exposed to a murine antigen (11% to 27% of children in inner cities in the United States are sensitized to mouse allergen).[48] Furthermore, different mechanisms may be involved in grade 4 reactions than in grade 1-3 reactions, since the time course appears to differ between the two. Data on rechallenged patients who experienced mild-to-moderate reactions supported a lack of IgE-mediated effect; however, rechallenge data for severe reactions are sparse.
Management of Infusion Reactions
FIGURE 2

Algorithm for the Treatment of Acute Anaphylactic Reactions
Mild-to-moderate infusion reactions are managed by slowing the infusion rate and by continuing antihistamine use prior to subsequent doses.[7] Grade 3 reactions also have been managed with continued antihistamine prophylaxis and a slowed infusion time.[47]
Severe infusion-related reactions associated with cetuximab require immediate and permanent discontinuation of cetuximab. Appropriate emergency medical therapy that includes epinephrine, corticosteroids, IV antihistamines, bronchodilators, and oxygen must be immediately available in the infusion suite or at bedside. Patients should be observed carefully until all signs and symptoms completely resolve.[7]
Recommendations for the diagnosis, follow-up, and management of acute anaphylactic reactions are available from the Joint Council of Allergy, Asthma and Immunology (JCAAI; Figure 2).[35] Specific pharmaceutical therapy for these reactions as recommended by the JCAAI is described in Table 4.[35] The most important element is immediate availability of epinephrine when agents associated with acute infusion-related anaphylactic or anaphylactoid reactions are administered.
To respond effectively to a cetuximab-related reaction, first, all medical staff caring for patients must be adequately trained in handling severe acute reactions. Second, standard order forms and protocols that address specific management techniques should be instituted. These documents should describe potentially life-threatening reactions (signs and symptoms to monitor and consider), standard orders that outline possibly necessary drugs and dosages and supportive measures (eg, intravenous fluids, oxygen), and follow-up measures (eg, monitoring for late reaction, patient education).
TABLE 4

Joint Council of Allergy, Asthma and Immunology Recommendations for the Pharmaceutical Management of Acute Anaphylaxis in Adults
Prophylactic measures (eg, administration of a histamine H1 antagonist given before each antibody dose) also should be instituted.[7] Diphenhydramine is the antihistamine most commonly used, although newer-generation, nonsedating options (ie, cetirizine [Zyrtec], loratadine [Claritin], or desloratadine [Clarinex]) may be considered; all of these newer drugs are available in syrup form for more rapid oral absorption.
Premedication does not always prevent reactions and does not preclude the need to prepare for management of severe reactions. When using cetuximab for the first time, it may be prudent to treat patients in a carefully controlled setting. Alternatively, physicians may work with a clinician with experience in managing such reactions (eg, an allergist).
Practical Considerations
Two key questions concerning preventing and treating severe acute infusion-related reactions remain unanswered. First, how do we identify patients at risk for a reaction? Second, when (and how) is it appropriate to rechallenge patients?
There is little available data about cetuximab that may help to answer these questions, although some data from the literature with other agents are of interest. No fail-safe method of identifying patients at risk for severe infusion-related reactions with other agents currently exists, but some risk factors, including an atopic history, female gender, concomitant medications, and comorbidities, have been identified. Other risk factors for morbidity and mortality associated with anaphylaxis are the presence of multiple antibiotic sensitivities and treatment with beta-adrenergic blocking agents or angiotensin-converting enzyme inhibitors.[35] Another important risk factor found among patients who suffered deadly reactions while receiving trastuzumab was preexisting, severe, malignancy-related respiratory distress.[27] While of interest, none of these risk factors has been studied consistently in the general context of monoclonal antibodies, and further data are welcomed.
It may be difficult for physicians to decide upon the timing of rechallenge, particularly after a severe reaction occurs. Data from trastuzumab and infliximab studies suggest that the majority of patients who develop severe reactions ultimately may continue therapy.[27,43] However, the risk of another reaction is still present and of concern. In many cases, both the clinician and patient must choose between a possible repeat reaction and withdrawal of a medication that may improve survival in a life-threatening disease.
When rechallenge is the preferred option, either a desensitization protocol or a graded challenge may be employed. Desensitization renders effector cells less reactive or nonreactive to IgE-mediated immune responses by rapid administration of incremental doses of an allergenic substance. In many cases, positive skin tests to the drug weaken or become negative. Biologic infusion reactions may not be IgE-mediated, but desensitization has been used anecdotally and successfully to retreat patients with this class of agents.
Graded challenge is a test dosing procedure that may be used in patients with a history of a non-IgE-mediated adverse reaction that begins with the administration of a small dose of the drug followed by progressive increases at regular intervals until a full dose is achieved. Depending on the drug used and the patient's response threshold, graded challenge with biologic agents may be completed within hours.
Neither procedure should be attempted before a skin-prick test is conducted by a person with training and experience (ie, an allergist). If the test is negative, a rechallenge procedure may be attempted. Desensitization or graded challenges with biologic agents should take no more than 1 day and must be performed in an intensive-care or step-down unit with one-to-one nursing, lifesaving equipment, and personnel who are readily available and appropriately trained.
Ultimately, the reactions associated with cetuximab must be specifically understood. To advance this goal in the setting of clinical trials, investigators should collect such data as assays for antigen-specific IgE, IgG, and other protein coaggregates and a broad survey of cytokines and vasoactive substances (C3a, C5a, histamine), serum tryptase levels (indicative of mast cell activation), and perhaps circulating EGFR, since immune aggregates may cause anaphylactoid reactions. When evaluating tryptase and IgE levels in patients who have suffered a reaction, 2-hour postinfusion samples should be collected and matched with control samples collected 2 hours after infusion from patients who have not had a reaction. Centralized measurements will decrease variability.
Other data that may prove interesting are patient atopy/allergy history, pretreatment skin testing for murine or other allergens that are components of cetuximab, and rechallenge data. A specific rechallenge study should be conducted, beginning with evaluating readministration to patients who developed grade 2/3 reactions before addressing more severe reactions. Finally, genotype analysis of patients who react may elucidate both pharmacogenetic predictors and etiologic factors.
Summary
Cetuximab, an anti-EGFR monoclonal antibody, is valuable in treating advanced colorectal cancer in chemorefractory patients. Its overall safety profile is favorable, because cetuximab does not elicit many adverse events traditionally associated with cytotoxic agents. Its most common side effect is an acneiform rash that results from its mechanism of action.
Severe infusion reactions resembling anaphylaxis occur in up to 4% of patients treated with cetuximab. Fatalities have occurred in less than 0.1% of patients treated with the monoclonal antibody. Therefore, these events are of significant concern for clinicians, as the symptoms may appear and progress very rapidly.
Currently, our understanding of the mechanism of these reactions is based on observations with the use of other agents. These reactions appear not to be IgE-mediated, given their prevalence with the first infusion. Limited data support this theory. However, variable mechanisms such as those seen with reactions to radiographic contrast material may be involved. Additional research is needed to understand the infusion-related reactions associated with cetuximab.
Acute, severe reactions to cetuximab may be managed with methods already described in the literature for anaphylactic reactions. The most important aspect of management is having epinephrine readily available. Other therapeutic modalities that may be required include antihistamines, bronchodilators, corticosteroids, oxygen, IV fluids, and vasopressors. The use of standard orders and protocols within the clinic will allow immediate, proper administration of therapy to help control the severity of these reactions.
Financial Disclosure:Dr. Patel is a consultant for Bristol-Myers Squibb, and preparation of this manuscript was supported by a grant from Bristol-Myers Squibb. Dr. Patel is currently Head, Autoimmunity & Transplantation Research at the Novartis Institutes for BioMedical Research in Basel, Switzerland.
References:
1. Maurizi M, Almadori G, Ferrandina G, et al: Prognostic significance of epidermal growth factor receptor in laryngeal squamous cell carcinoma. Br J Cancer 74:1253-1257, 1996.
2. Mayer A, Takimoto M, Fritz E, et al: The prognostic significance of proliferating cell nuclear antigen, epidermal growth factor receptor, and mdr gene expression in colorectal cancer. Cancer 71:2454-2460, 1993.
3. Messa C, Russo F, Caruso MG, et al: EGF, TGF-alpha, and EGF-R in human colorectal adenocarcinoma. Acta Oncol 37:285-289, 1998.
4. Rubin Grandis J, Melhem MF, Barnes EL, et al: Quantitative immunohistochemical analysis of transforming growth factor-alpha and epidermal growth factor receptor in patients with squamous cell carcinoma of the head and neck. Cancer 78:1284-1292, 1996.
5. Cunningham D, Humblet Y, Siena S, et al: Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med 351:337-345, 2004.
6. Bonner JA, Giralt J, Harari P, et al: Cetuximab prolongs survival in patients with locoregionally advanced squamous cell carcinoma of head and neck: A phase III study of high dose radiation therapy with or without cetuximab (abstract 5507). J Clin Oncol 22(suppl):488, 2004.
7. Erbitux (cetuximab) [package insert]. Princeton, NJ; Bristol-Myers Squibb Co; 2005.
8. National Cancer Institute-Cancer Therapy Evaluation Program: CTCAE v3.0. Available at http://ctep.cancer.gov/reporting/ctc.html. Accessed November 29, 2005.
9. Lenz HJ, Mayer RJ, Gold PJ, et al: Activity of cetuximab in patients with colorectal cancer refractory to both irinotecan and oxaliplatin (abstract 3510). Proc Am Soc Clin Oncol 23:248, 2004.
10. Saltz LB, Meropol NJ, Loehrer PJ Sr, et al: Phase II trial of cetuximab in patients with refractory colorectal cancer that expresses the epidermal growth factor receptor. J Clin Oncol 22:1201-1208, 2004.
11. Saltz L, Kies M, Abbruzzese JL, et al: The presence and intensity of the cetuximab-induced acne-like rash predicts increased survival in studies across multiple malignancies (abstract 817). Proc Am Soc Clin Oncol 22:204, 2003.
12. Saltz LB, Lenz HJ, Kindler H, et al: Interim report of randomized phase II trial of cetuximab/bevacizumab/irinotecan (CBI) versus cetuximab/bevacizumab (CB) in irinotecan-refractory colorectal cancer (abstract 169b). American Society of Clinical Oncology 2005 Gastrointestinal Cancer Symposium. Available at wwww.asco.org. Accessed September 13, 2006.
13. Perez-Soler, Saltz L: Cutaneous adverse effects with HER1/EGFR-targeted agents: is there a silver lining? J Clin Oncol 23:5235-5246, 2005.
14. Burtness BA, Li Y, Flood W, et al: Phase III trial comparing cisplatin (C) + placebo (P) to C + anti-epidermal growth factor antibody (EGF-R) C225 in patients (pts) with metastatic/recurrent head & neck cancer (HNC) (abstract 901). Proc Am Soc Clin Oncol 21:226a, 2002.
15. Rosell R, Daniel C, Ramlau R, et al: Randomized phase II study of cetuximab in combination with cisplatin and vinorelbine vs. cisplatin/vinorelbine alone in the first-line treatment of patients (pts) with epidermal growth factor receptor-expressing advanced non-small-cell lung cancer (abstract 7012). Proc Am Soc Clin Oncol 23:618, 2004.
16. Van Laan S: United States Adopted Names: Monoclonal antibodies. April 11, 2005. Available from American Medical Association at www.ama-assn.org/ama/pub/category/13280.html. Accessed November 29, 2005.
17. Dillman RO: Monoclonal antibodies for treating cancer. Ann Intern Med 111:592-603, 1989.
18. Avner B, Swindell L, Sharp E, et al: Evaluation and clinical relevance of patient immune responses to intravenous therapy with murine monoclonal antibodies conjugated to adriamycin. Mol Biother 3:14-21, 1991.
19. Goodman GE, Hellstrom I, Brodzinsky L, et al: Phase I trial of murine monoclonal antibody L6 in breast, colon, ovarian, and lung cancer. J Clin Oncol 8:1083-1092, 1990.
20. Sears HF, Atkinson B, Mattis J, et al: Phase-I clinical trial of monoclonal antibody in treatment of gastrointestinal tumours. Lancet 1:762-765, 1982.
21. Morrison SL, Johnson MJ, Herzenberg LA, et al: Chimeric human antibody molecules: Mouse antigen-binding domains with human constant region domains. Proc Natl Acad Sci U S A 81:6851-6855, 1984.
22. Riechmann L, Clark M, Waldmann H, et al: Reshaping human antibodies for therapy. Nature 332:323-327, 1988.
23. Jones PT, Dear PH, Foote J, et al: Replacing the complementarity-determining regions in a human antibody with those from a mouse. Nature 321:522-525, 1986.
24. Burtrum D, Zhu Z, Lu D, et al: A fully human monoclonal antibody to the insulin-like growth factor I receptor blocks ligand-dependent signaling and inhibits human tumor growth in vivo. Cancer Res 63:8912-8921, 2003.
25. Herceptin (trastuzumab) [package insert]. South San Francisco; Genentech, Inc; 2005.
26. Humira (adalimumab) [package insert]. North Chicago, Abbott Laboratories; 2004.
27. Cook-Bruns N: Retrospective analysis of the safety of Herceptin immunotherapy in metastatic breast cancer. Oncology 61:58-66, 2001.
28. Present DH, Rutgeerts P, Targan S, et al: Infliximab for the treatment of fistulas in patients with Crohn's disease. N Engl J Med 340:1398-1405, 1999.
29. Coiffier B, Lepage E, Brière J, et al: CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346:235-242, 2002.
30. Remicade (infliximab) [package insert]. Malvern, Pa; Centocor, Inc; 2004.
31. Rituxan (rituximab) [package insert]. South San Francisco; Genentech, Inc; 2005.
32. Taxol (paclitaxel) [package insert]. Princeton, NJ; Bristol-Myers Squibb Co; 2003.
33. Eloxatin (oxaliplatin for injection) [package insert]. New York; Sanofi-Synthelabo Inc; 2004.
34. Paraplatin (carboplatin aqueous solution) [package insert]. Princeton, NJ; Bristol-Myers Squibb Co; 2004.
35. Lieberman P, Kemp SF, Oppenheimer J: The diagnosis and management of anaphylaxis: an updated practice primer. Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology J Allergy Clin Immunol 115:S483-S523, 2005.
36. Gruchalla RS: Drug allergy. J Allergy Clin Immunol 111(2 suppl):S548-S559, 2003.
37. Ennis M, Lorenz W, Kapp B, et al: Comparison of the histamine-releasing activity of cremophor E1 and some of its derivatives in two experimental models: The in vivo anaesthetized dog and in vitro rat peritoneal mast cells. Agents Actions 16:265-268, 1985.
38. Itoh Y, Sendo T, Hirakawa T, et al: Role of sensory nerve peptides rather than mast cell histamine in paclitaxel hypersensitivity. Am J Respir Crit Care Med 169:113-119, 2004.
39. Weiss RB, Donehower RC, Wiernik PH, et al: Hypersensitivity reactions from taxol. J Clin Oncol 8:1263-1268, 1990.
40. Markman M, Kennedy A, Webster K, et al: Paclitaxel-associated hypersensitivity reactions: Experience of the gynecologic oncology program of the Cleveland Clinic Cancer Center. J Clin Oncol 18:102-105, 2000.
41. Thomas RR, Quinn MG, Schuler B, et al: Hypersensitivity and idiosyncratic reactions to oxaliplatin. Cancer 97:2301-2307, 2003.
42. Gowda A, Goel R, Berdzik J, et al: Hypersensitivity reactions to oxaliplatin: Incidence and management. Oncology (Williston Park, NY) 18:1671-1675, 2004.
43. Cheifetz A, Smedley M, Martin S, et al: The incidence and management of infusion reactions to infliximab: A large center experience. Am J Gastroenterol 98:1315-1324, 2003.
44. Laroche D, Namour F, Lefrancois C, et al: Anaphylactoid and anaphylactic reactions to iodinated contrast material. Allergy 54:13-16, 1999.
45. Shin DM, Donato NJ, Perez-Soler R, et al: Epidermal growth factor receptor-targeted therapy with C225 and cisplatin in patients with head and neck cancer. Clin Cancer Res 7:1204-1213, 2001.
46. Needle MN: Safety experience with IMC-C225, an anti-epidermal growth factor receptor antibody. Semin Oncol 29:55-60, 2002.
47. Robert F, Ezekiel MP, Spencer SA, et al: Phase I study of anti-epidermal growth factor receptor antibody cetuximab in combination with radiation therapy in patients with advanced head and neck cancer. J Clin Oncol 19:3234-3243, 2001.
48. Phipatanakul W, Eggleston PA, Wright EC, et al: Mouse allergen. II. The relationship of mouse allergen exposure to mouse sensitization and asthma morbidity in inner-city children with asthma. J Allergy Clin Immunol 106:1075-1080, 2000.