Chemo/Immunotherapy Confers Greater Therapy-Related MDS/AML Risk in Survivors
Investigators note that although therapy-related myelodysplastic syndromes or acute myeloid leukemia are not common, efforts to reduce treatment-associated toxicity in survivors of lymphoid neoplasms are needed given the poor prognosis associated with the diagnosis.
"With further advances in therapeutic approaches for lymphoid neoplasms, future studies with additional follow-up, newer therapies, and detailed clinical data will be important for assessing [therapy-related] MDS/AML risks and informing evolving risk/benefit assessments for specific treatment regimens," according to the study authors.
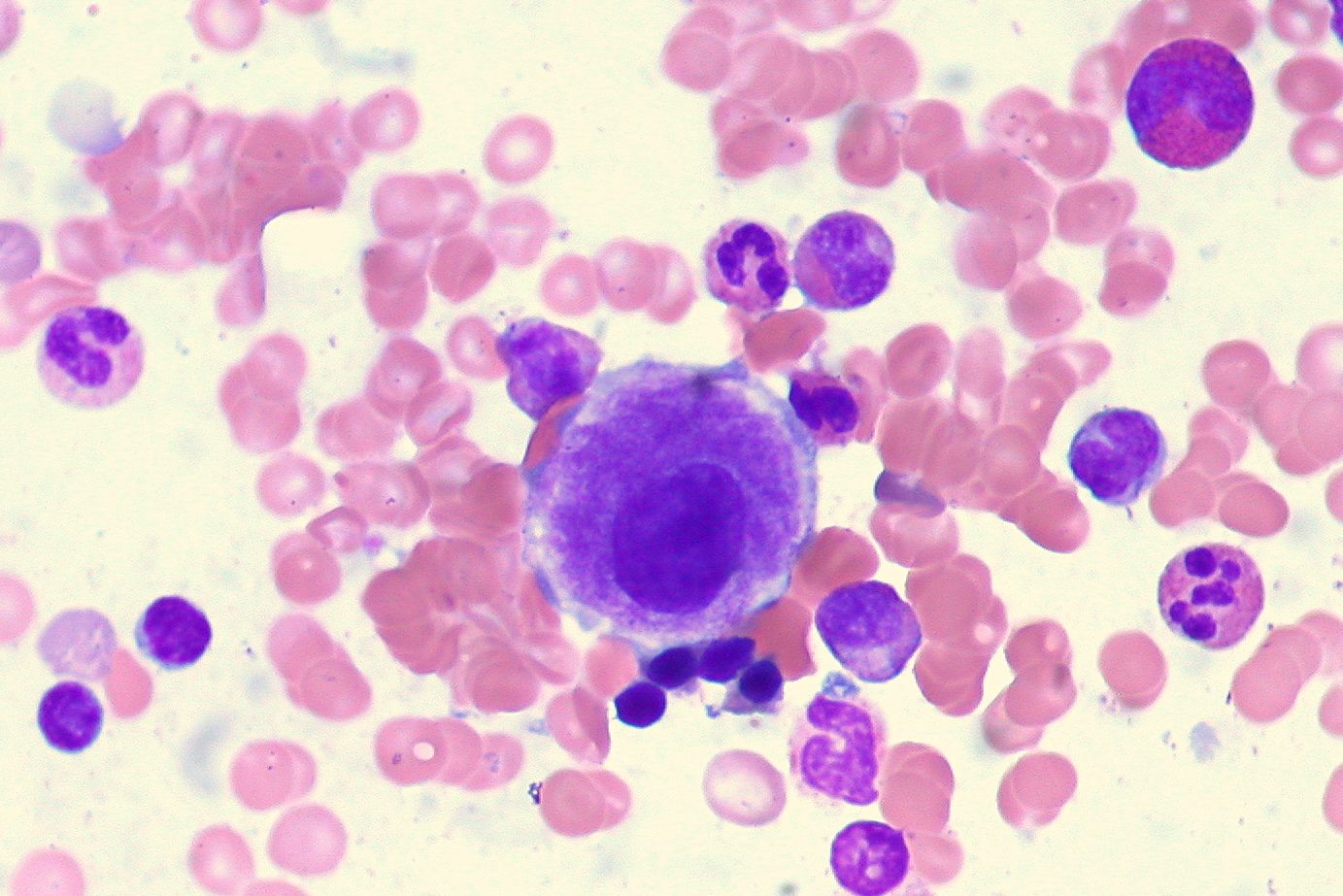
Survivors of lymphoid neoplasms who received initial chemotherapy or immunotherapy may have a higher risk of developing therapy-related myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML), although those treated more recently generally had a lower risk, according to findings from a study published in The Lancet.
There were 1496 instances of therapy-related MDS/AML diagnosed during a median follow-up of 3.9 years (interquartile range [IQR], 1.5-8.1). The incidence rate of therapy-related MDS/AML was 6.4 times (95% CI, 6.1-6.7) higher than what was expected in the general population. Moreover, investigators noted an excess absolute risk (EAR) of 12.8 instances per 10,000 person-years.
Investigators observed an elevated risk of therapy-related MDS/AML following initial chemotherapy or immunotherapy for patients with precursor leukemia/lymphoma (standardized incidence ratio [SIR], 39; EAR, 30), Burkitt leukemia/lymphoma (SIR, 20; EAR, 24), peripheral T-cell lymphoma (PTCL; SIR, 12; EAR, 23), and chronic lymphocytic leukemia (CLL) or small lymphocytic leukemia (SLL; SIR, 9.0; EAR, 27). There were also elevated risks after initial treatment for Hodgkin lymphoma, follicular lymphoma, plasma cell neoplasms, diffuse large B-cell lymphoma (DLBCL), and marginal zone lymphoma (MZL; SIRs, 4.2-6.9; EARs, 4.9-15.0).
In an analysis of 10-year cumulative incidence rates of therapy-related MDS/AML, the highest risks were for patients receiving treatment for Burkitt leukemia/lymphoma (2.0%), CLL/SLL (1.9%), mantle cell lymphoma (MCL; 1.7%), precursor leukemia/lymphoma (1.4%), and PTCL (1.4%). Moreover, the median survival following therapy-related MDS/AML was 8.0 months (IQR, 3.0-22.0).
“Despite the rarity of [therapy-related] MDS/AML, the 8-month median survival after [therapy-related] MDS/AML diagnosis emphasizes the high fatality rate of this rare outcome,” the study authors wrote. “With further advances in therapeutic approaches for lymphoid neoplasms, future studies with additional follow-up, newer therapies, and detailed clinical data will be important for assessing [therapy-related] MDS/AML risks and informing evolving risk/benefit assessments for specific treatment regimens.”
Patients who received initial treatment for CLL/SLL experienced a higher risk of therapy-related MDS/AML when treated more recently compared with those receiving treatment earlier in the study period (SIR2000-2005, 4.8; SIR2006-2011, 13; SIR2012-2017, 10; Ptrend = .0043). This risk declined significantly for patients who received more recent treatment for Hodgkin lymphoma (SIR2000-2005, 15; SIR2006-2011, 7.1; SIR2012-2017, 6.3; Ptrend = .024); the same was true for patients with MZL (SIR2000-2005, 7.5; SIR2006-2011, 4.6; SIR2012-2017, 2.3; Ptrend = .015).
Investigators noted lower SIRs for therapy-related MDS/AML risk in the most recent calendar period of 2012 to 2017 for patients with MCL (Ptrend = .054), lymphoblastic lymphoma or Waldenström macroglobulinemia (Ptrend = .067), and plasma cell neoplasms (Ptrend = .051). Additionally, there was no temporal change in risk for therapy-related MDS/AML in patients receiving initial therapy for DLBCL (Ptrend = .025).
The 5-year cumulative incidence of therapy-related MDS/AML increased from 0.49% during 2000 to 2005 to 1.5% during 2006 to 2011 and 1.1% during 2012 to 2017 for patients treated for CLL/SLL. For patients with Hodgkin lymphoma, the 5-year cumulative incidence rate was 0.38% during 2000 to 2005, 0.22% during 2006 to 2011, and 0.20% during 2012 to 2017. For those with MZL, the 5-year rate was 0.71% during 2000 to 2005, 0.47% during 2006 to 2011, and 0.19% during 2012 to 2017.
Investigators of this study assessed data from patients diagnosed with a first primary lymphoid malignancy at ages 20 to 84 from 2000 to 2017 who survived at least 1 year following diagnosis without developing a second malignancy and received initial chemotherapy or immunotherapy. These data came from 17 National Cancer Institute Surveillance, Epidemiology, and End Results cancer registry areas that made up 27.8% of the United States population. Investigators did not include data from patients under the age of 20, as treatment approaches may have differed for pediatric patients.
Investigators quantified the observed or expected relative risk of therapy-related MDS/AML occurrence compared with that expected in the general population using SIRs. Other measures included EARs or the observed/expected risk per 10,000 person-years, cumulative incidence of therapy-related MDS/AML, and median survival following therapy-related MDS/AML.
The study cohort included 186,503 patients who received initial chemotherapy or immunotherapy. At least 67% of those with first primary Hodgkin lymphoma, precursor leukemia/lymphoma, Burkitt leukemia/lymphoma, MCL, DLBCL, hairy cell leukemia, and plasma cell neoplasms received initial treatment. Moreover, less than 35% of those with CLL/SLL and MZL received initial treatment.
Median patient ages at diagnosis ranged from 53.5 to 67.5 years outside of those with Hodgkin lymphoma (37.5 years; IQR, 27.5-51.5), precursor leukemia/lymphoma (40.5 years; IQR, 28.5-54.5), and Burkitt leukemia/lymphoma (45.5 years; IQR, 34.5-57.5). Initial therapy also most commonly included radiotherapy for those with Hodgkin lymphoma (34.3%), precursor leukemia/lymphoma (26.2%), DLBCL (25.8%), and plasma cell neoplasms (22.9%).
Reference
Morton LM, Curtis RE, Linet MS, et al. Trends in risk for therapy-related myelodysplastic syndrome/acute myeloid leukemia after initial chemo/immunotherapy for common and rare lymphoid neoplasms, 2000–2018. EClinicalMedicine. 2023;61:102060 doi:10.1016/j.eclinm.2023.102060
How Supportive Care Methods Can Improve Oncology Outcomes
Experts discussed supportive care and why it should be integrated into standard oncology care.
How Supportive Care Methods Can Improve Oncology Outcomes
Experts discussed supportive care and why it should be integrated into standard oncology care.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.