Epidemiology and Histopathology
Carcinoma of the urethra is uncommon, accounting for less than 1% of malignancies in men,[1] with fewer than 600 cases reported worldwide.[2,3] The average age at presentation is 58 to 60 years, although 10% of cases occur in men younger than 40 years of age.[4] Although clear etiologic factors have not been identified, there seems to be a correlation between the incidence of urethral cancer and conditions causing chronic irritation or inflammation, such as sexually transmitted diseases, strictures, trauma, or urethritis.[5] A significant percentage of men with urethral cancer have a history of occupational exposure to smoking and other known carcinogens that affect the bladder and upper urinary tract.[2,6] Patients most commonly present with obstructive symptoms.[4] Other presenting signs and symptoms include mass, dysuria, discharge, pain, and hematuria. The interval between onset of symptoms to diagnosis may be as long as 3 years,[7] mainly because of failure to seek medical consultation or misdiagnosis of the condition, with most symptoms often attributed to urethritis or urethral stricture.[6] Survival of patients with lower-stage tumors primarily treated with surgery has been reported to range from 67% to 100%, whereas survival of men with more advanced urethral cancer is reported to range from 33% to 44%.[4,8,9]
Histologically, there are both superficial glandular tubules as well as stratified squamous epithelium, pseudostratified columnar epithelium, and urothelial (transitional) epithelium along the urethra. As a result, although the most common histology in urethral carcinoma is squamous cell carcinoma (occurring in up to 80% of cases), men may also present with urothelial carcinoma (in 20% to 33% of cases) and adenocarcinoma (in < 5% of cases).[4,10]
Anatomy and Lymphatic Drainage
The male urethra can be divided into three regional segments: prostatic, membranous, and penile. The posterior urethra is composed of the membranous and prostatic segments. The anterior urethra is composed of the penile urethra, with its bulbar and pendulous segments.[11] However, many authors describe the bulbar region as being posterior because its behavior is similar to that of the membranous urethra. The bulbomembranous urethra is most commonly affected by carcinoma (59% of cases), followed by the pendulous urethra (33% of cases) and the prostatic urethra (7% of cases), with posterior tumors having a worse prognosis compared with those arising from the anterior urethra.[4,10]
The penile urethra is drained by lymphatics that accompany those of the glans penis, which drain into the deep inguinal and external iliac lymphatic chains. In contrast, the bulbomembranous and prostatic segments of the urethra drain through three lymphatic channels into the pelvis. The first extends along the dorsal vein of the penis through the external iliac nodes. The second extends along the pudendal artery to the obturator and internal iliac lymph nodes. The third joins the presacral lymphatic drain.[12]
Surgical Treatment
Historically, the primary mode of treatment for male urethral carcinoma has been surgical excision. Previous studies have assessed the use of local excision, partial penectomy, radical penectomy, or cystoprostatectomy with penectomy.[13] Conservative therapy with local excision is rarely offered, due to the aggressive nature of the disease, although this approach could be considered in patients who are not candidates for more traditional treatment because of a concomitant medical problem or refusal of traditional methods.
Cystoprostatectomy with penectomy generally involves an en bloc resection that could encompass the inferior pubic rami, prostate, bladder, penis, and perineum. It has been used in at least 11 studies; 25 of the 64 (38%) patients were free of disease for various periods of time.[5,13-20] Because of the extensive nature of the resection, authors have reported complications ranging from perineal hernia and pelvic abscesses, to postoperative death.[15,21] Other disadvantages to cystoprostatectomy with penectomy include lack of organ preservation and morbidity from a radically disfiguring operation. As a result of the disfiguring nature of cystoprostatectomy with penectomy, many men are reluctant to undergo en bloc resection.
Recommended Treatment Paradigm
Patients with urothelial carcinoma who present as candidates for consideration of chemoradiation therapy have typically been offered surgical intervention but refused the proposed procedure. Physical examination and staging (with contrast-enhanced computed tomography [CT] scan of the abdomen and pelvis) is needed to determine extent of disease and to rule out metastases that would preclude locally aggressive treatment. Cystourethroscopy is necessary for histopathologic confirmation and maximal transurethral resection. Because urethral cancers can be difficult to see on a typical CT simulation scan, magnetic resonance imaging (MRI) is often obtained to aid with radiation treatment planning. MRI is also useful, along with regular cystoscopic examination, for post-treatment surveillance; for this reason, it is good to have a baseline scan for comparative purposes. After initial workup and staging, the patient should be seen not only by the diagnosing urologist and radiation oncologist, but also by a medical oncologist specializing in genitourinary cancers. In addition, his case should be discussed by a multidisciplinary tumor board. The patient should be warned that chemoradiation of the urethra and its draining lymphatics is a difficult treatment to endure, but most patients are highly motivated given the alternatives.
When the chemoradiotherapy regimen has been decided (typically radiation concurrent with weekly cisplatin, or fluorouracil [5-FU] plus mitomycin-C), CT simulation for treatment planning is performed. Given the large volumes potentially irradiated, and the need to protect critical structures and surrounding normal tissue, intensity-modulated radiation therapy is preferred. During radiation treatment planning, a CT simulation scan is performed with the patient lying in a custom body mold. If inguinal lymph nodes are to be targeted, or if the penile urethra is involved, a radiation bolus material can be used to increase the superficial radiation dose, and the penis must be reproducibly positioned in a custom mold.
Since patients undergoing irradiation for urethral cancer are at high risk for urethral strictures or obstruction from tumor and epithelial sloughing, an indwelling bladder catheter can be placed, to remain in the patient throughout the course of radiation therapy. Undergoing radiotherapy with an indwelling urethral catheter in place is extremely irritating, so the use of topical bladder anesthetics such as phenazopyridine or the instillation of lidocaine by the urologist can be very helpful. Alternatively, for patients who want to avoid catheterization, a scheduled cystoscopy every 2 to 3 weeks during treatment can be helpful to prevent obstruction and allow treatment response to be monitored. For this reason, multidisciplinary care and communication between the radiation oncologist, urologist, and medical oncologist is critical.
For patients with an anterior urethral carcinoma not involving the bulbomembranous urethra, irradiation of groin nodes in addition to the tumor can be considered. Lymph node chains at risk can be irradiated to 45 Gy in 1.8-Gy fractions in combination with chemotherapy, taking care to respect the radiation tolerance of the small bowel. A total dose of 66.6 Gy, administered in 1.8-Gy fractions, can be delivered to the primary tumor. For tumors of the prostatic portion of the urethra that do not involve the bulbomembranous segment, the pelvic lymph nodes (internal and external iliac, and presacral lymph node chains) and primary tumor can be targeted. For any tumors that encompass both the anterior and posterior urethra, or involve the bulbomembranous urethra, both the inguinal and pelvic lymph node chains will need to be treated, in addition to the primary tumor. Given the critical need for reproducible treatment, daily image guidance is recommended to ensure correct positioning.
KEY POINTS
- Surgical treatment for urethral carcinoma is often disfiguring. It is reasonable to offer chemoradiotherapy to patients for organ preservation.
- Due to its rarity, standard treatment paradigms for urethral carcinoma are not robustly established. Depending on the histology of the tumor, the physician can offer chemoradiation employing regimens used for urothelial or squamous cell carcinoma of the bladder.
- Regional irradiation fields should take into consideration the lymphatic drainage of the involved urethra.
Unfortunately, since recurrence is not uncommon, careful post-treatment surveillance is required. Within the first year post treatment, a cystoscopy can be performed at 1, 3, and 6 months, and an MRI scan should be done at 6 and 12 months. Post-treatment surveillance after the first year can involve physical examination, yearly cystoscopy, and MRI. If the tumor does not regress or recurs, salvage surgery is the only potentially curative option. Patients should be counseled that the likelihood of erectile dysfunction following such surgery is high. If the prostate and external urinary sphincter are within the high-dose radiotherapy region, stress incontinence is possible.
Review of the Literature
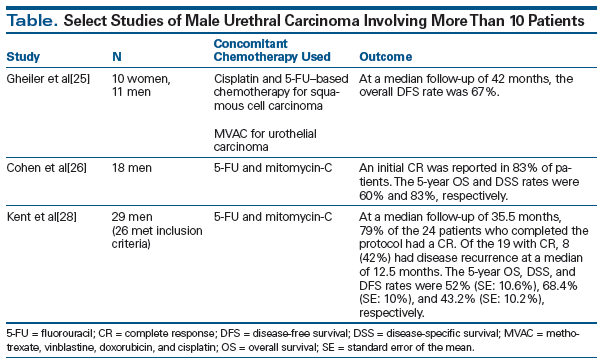
Concomitant chemoradiation has been investigated in trials with small numbers of patients, and the results have been encouraging. Studies have reported increases in long-term survival (with a 5-year disease-specific survival rate of 83% in one study) among patients treated with an integrated approach of concurrent chemoradiation or concurrent chemoradiation followed by surgery.[22-28] In 1992, Baskin and Turzan described the first case of male urethral carcinoma that resulted in pathological remission with sustained remission at 2.5 years; the patient had been treated with combined 5-FU and mitomycin-C and simultaneous irradiation to the tumor at 40 Gy in 20 fractions over a 4-week period, followed by urethral resection.[22] More recent studies that include more than 10 patients have reported promising results with chemoradiation as well (see Table).[25,26,28]
Conclusion
More research is needed to define the optimal radiotherapy and chemotherapy regimen for male urethral carcinoma. However, modern chemoradiation is a feasible treatment option for motivated men with urethral carcinoma who want to preserve their organs.
Financial Disclosure: The authors have no significant financial interest in or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Swartz MA, Porter MP, Lin DW, Weiss NS. Incidence of primary urethral carcinoma in the United States. Urology. 2006;68:1164-8.
2. Forman JD, Lichter AS. The role of radiation therapy in the management of carcinoma of the male and female urethra. Urol Clin North Am. 1992;19:383-9.
3. Levine RL. Urethral cancer. Cancer. 1980;45:1965-72.
4. Dalbagni G, Zhang ZF, Lacombe L, Herr HW. Male urethral carcinoma: analysis of treatment outcome. Urology. 1999;53:1126-32.
5. Kaplan GW, Bulkey GJ, Grayhack JT. Carcinoma of the male urethra. J Urol. 1967;98:365-71.
6. Mansur DB. Cancer of the penis and male urethra. In: Halperin EC, Perez CA, Brady LW, Wazer DE, editors. Principles and practice of radiation oncology, sixth ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013. p. 1345-54.
7. Mostofi FK, Davis CJ Jr, Sesterhenn IA. Carcinoma of the male and female urethra. Urol Clin North Am. 1992;19:347-58.
8. Dinney CP, Johnson DE, Swanson DA, et al. Therapy and prognosis for male anterior urethral carcinoma: an update. Urology. 1994;43:506-14.
9. Thyavihally YB, Tongaonkar HB, Srivastava SK, et al. Clinical outcome of 36 male patients with primary urethral carcinoma: a single center experience. Int J Urol. 2006;13:716-20.
10. Srinivas V, Khan SA. Male urethral cancer. A review. Int Urol Nephrol. 1988;20:61-5.
11. Carroll PR, Dixon CM. Surgical anatomy of the male and female urethra. Urol Clin North Am. 1992;19:339-46.
12. Hand JR. Surgery of the penis and urethra. In: Campbell MF, Harrison JH, editors. Urology, third ed. Philadelphia, PA: WB Saunders; 1970. p. 2541-647.
13. Zeidman EJ, Desmond P, Thompson IM. Surgical treatment of carcinoma of the male urethra. Urol Clin North Am. 1992;19:359-72.
14. Mandler JI, Pool TL. Primary carcinoma of the male urethra. J Urol. 1966;96:67-72.
15. Klein FA, Whitmore WF Jr, Herr HW, et al. Inferior pubic rami resection with en bloc radical excision for invasive proximal urethral carcinoma. Cancer. 1983;51:1238-42.
16. King LR. Carcinoma of the urethra in male patients. J Urol. 1964;91:555-9.
17. Howe GE, Prentiss RJ, Mullenix RB, Feeney MJ. Carcinoma of the urethra: diagnosis and treatment. J Urol. 1963;89:232-5.
18. Hotchkiss RS, Amelar RD. Primary carcinoma of the male urethra. J Urol. 1954;72:1181-91.
19. Bracken RB, Henry R, Ordonez N. Primary carcinoma of the male urethra. South Med J. 1980;73:1003-5.
20. Anderson KA, McAninch JW. Primary squamous cell carcinoma of anterior male urethra. Urology. 1984;23:134-40.
21. Shuttleworth KE, Lloyd-Davies RW. Radical resection for tumours involving the posterior urethra. Br J Urol. 1969;41:739-43.
22. Baskin LS, Turzan C. Carcinoma of male urethra: management of locally advanced disease with combined chemotherapy, radiotherapy, and penile-preserving surgery. Urology. 1992;39:21-5.
23. Licht MR, Klein EA, Bukowski R, et al. Combination radiation and chemotherapy for the treatment of squamous cell carcinoma of the male and female urethra. J Urol. 1995;153:1918-20.
24. Oberfield RA, Zinman LN, Leibenhaut M, et al. Management of invasive squamous cell carcinoma of the bulbomembranous male urethra with co-ordinated chemo-radiotherapy and genital preservation. Br J Urol. 1996;78:573-8.
25. Gheiler EL, Tefilli MV, Tiguert R, et al. Management of primary urethral cancer. Urology. 1998;52:487-93.
26. Cohen MS, Triaca V, Billmeyer B, et al. Coordinated chemoradiation therapy with genital preservation for the treatment of primary invasive carcinoma of the male urethra. J Urol. 2008;179:536-41.
27. Itoh J, Mitsuzuka K, Kimura S, et al. Docetaxel, cisplatin and 5-fluorouracil chemotherapy with concurrent radiation for unresectable advanced urethral carcinoma. Int J Urol. 2014;21:422-4.
28. Kent M, Zinman L, Girshovich L, et al. Combined chemoradiation as primary treatment for invasive male urethral cancer. J Urol. 2015;193:532-7.