CML Stem Cell Burden at Diagnosis Associated With Treatment Outcomes
Contrary to previous laboratory findings, a new study has shown for the first time the effect of stem cell burden on treatment outcome, discovering that tyrosine kinase inhibitors, including imatinib and dasatinib, can rapidly eradicate most chronic myeloid leukemia stem cells.
Laboratory studies have suggested that chronic myeloid leukemia (CML) stem cells are resistant to tyrosine kinase inhibitor (TKI) treatment. A new study, though, showed for the first time the effect of stem cell burden on treatment outcome and actually found that TKIs, including imatinib and dasatinib, can rapidly eradicate most CML stem cells.
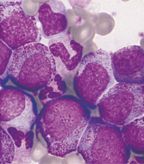
Photomicrograph of chronic myeloid leukemia, also known as myelogenous leukemia, from a blood smear; © Prof. Jean Bonhomme
The study, led by Satu Mustjoki, MD, PhD, of the University of Helsinki in Finland, was published online ahead of print in Leukemia in February. The phase II trial included 46 newly diagnosed CML patients; the researchers counted Philadelphia chromosome-positive (Ph+) leukemic stem cells (LSCs) and progenitor cells (LPCs), using flow cytometry and fluorescence in situ hybridization techniques.
The burden of LSCs varied widely among the patients, from 0.6% (meaning the majority of stem cells were Philadelphia chromosome-negative) all the way to 100%; the range of LPCs was tighter, at 57% to 100%. The median LSC burden was 79% vs 96% for LPCs (P = .0001). LSC count at diagnosis was correlated with leukocyte count, enlarged spleen size, and percentage of blasts in the peripheral blood.
A higher LSC burden at diagnosis appeared to have an effect on treatment-related toxicity. Patients in a “high group,” with greater than 79% LSCs, experienced more grade 2 or higher hematological toxicity during the first 3 months of TKI therapy compared with those in a “low group” (55% vs 19%, P = .024); this was primarily due to a difference in the rate of neutropenia.
The LSC burden also correlated with treatment response. “The proportion of Ph+ cells in the stem cell fraction at diagnosis correlated with the cytogenetic responses at 1 (r = 0.63, P < .0001), 3 (r = 0.48, P = .0025), and 6 months (r = 0.36, P = .0271),” the authors wrote. At 12 months, all patients with samples available for analysis (21 treated with dasatinib and 21 treated with imatinib) were in complete cytogenetic remission. In patients with high LSC burden at diagnosis, major molecular response was more likely in the dasatinib arm than the imatinib arm.
In both treatment groups, LSCs dropped precipitously, contrasting with the in vitro data from earlier work; by 6 months, both groups had 0% burden. Dasatinib did appear to deplete LPCs faster than imatinib, the authors noted.
“We speculate that CML patients with a high stem cell disease burden at the time of diagnosis have a more advanced or biologically more complex disease,” they wrote. “Accordingly, the LSC burden at diagnosis carried a strong prognostic value.” All patients in the study who did not achieve a major molecular response by 18 months had greater than 75% LSC burden at diagnosis.
“LSC burden is a novel prognostic biomarker and may be very useful in detecting high-risk patients who would benefit from treatment intensification,” the authors concluded.