Combined Lenalidomide/Rituximab Active in Recurrent Follicular Lymphoma
Combined treatment with lenalidomide/rituximab resulted in better clinical response in patients with recurrent follicular lymphoma than did lenalidomide alone.
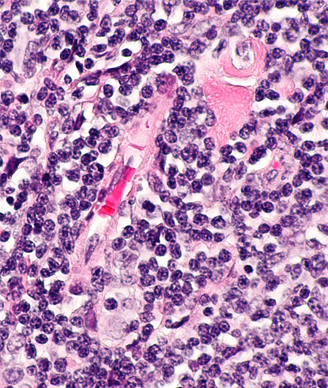
Micrograph showing a small B-cell lymphoma compatible with follicular lymphoma. Copyright © 2014 Nephron.
Combined treatment with lenalidomide and rituximab resulted in better clinical response in patients with recurrent follicular lymphoma than did treatment with lenalidomide alone, according to the results of a study published in the Journal of Clinical Oncology.
“Our group believes that the results from CALGB (Alliance) 50401 provide sufficient safety and efficacy data to support the use of lenalidomide/rituximab as a backbone to move toward combination biologic triplet therapy as we explore our next generation of chemotherapy-free regimens in indolent and other lymphomas,” wrote John P. Leonard, MD, of Weill Cornell Medical College and New York Presbyterian Hospital, and colleagues.
The monoclonal antibody rituximab is currently approved for the treatment of relapsed or refractory follicular lymphoma. According to the study, patients often initially respond but later relapse. Research has also explored the use of other drugs in combination with rituximab as a treatment method for patients who experience relapse.
In this phase II study, the researchers explored the use of rituximab in combination with the immunomodulatory drug lenalidomide. The trial initially assigned patients to rituximab alone, lenalidomide alone (n = 45), or combined rituximab/lenalidomide (n = 46); however, the rituximab alone arm was discontinued due to poor accrual.
Overall, study results showed that combined treatment with lenalidomide/rituximab had good clinical activity in patients with recurrent follicular lymphoma. Thirty-six percent of patients assigned lenalidomide and 63% of patients assigned the combination were able to complete 12 cycles of treatment.
The overall response rate was significantly higher for patients receiving lenalidomide/rituximab compared with lenalidomide alone (76% vs 53%; P = .029). Patients assigned lenalidomide/rituximab had a median time to progression of 2 years compared with 1.1 years for patients assigned lenalidomide alone (P = .0023).
Overall, patients assigned to both arms experienced similar toxicity; however, 22% of patients assigned lenalidomide discontinued therapy as a result of adverse events.
Grade 3/4 adverse events occurred in 58% of patients assigned lenalidomide and 53% of patients assigned to the combination. These adverse events included neutropenia (16% on lenalidomide vs 20% of the combination), fatigue (9% vs 13%), and thrombosis (16% vs 4%).
“Interestingly, there was a trend toward less thrombosis in the lenalidomide/rituximab arm, which we speculate may be a result of better lymphoma control, reducing venous obstruction and other risks for clot,” the researchers wrote. “It is important to stress that the heterogeneous nature of the patient population with respect to thrombosis risk (and associated use of aspirin and anticoagulants as prophylaxis) makes it difficult to assess the effectiveness of ancillary care measures in preventing this complication.”
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.