Complete Retroperitoneal Resection Appears Critical Vs RPLND in Testicular Cancer
Investigators report no differences in progression-free survival among patients with nonseminomatous testicular cancer who received surveillance or adjuvant chemotherapy in a cohort study.
In this retrospective cohort study, investigators collected data on 117 patients with nonseminomatous testicular cancer who received cisplatin-based frontline chemotherapy and underwent subsequent RPLND from 1990 to 2018 at 13 institutions.
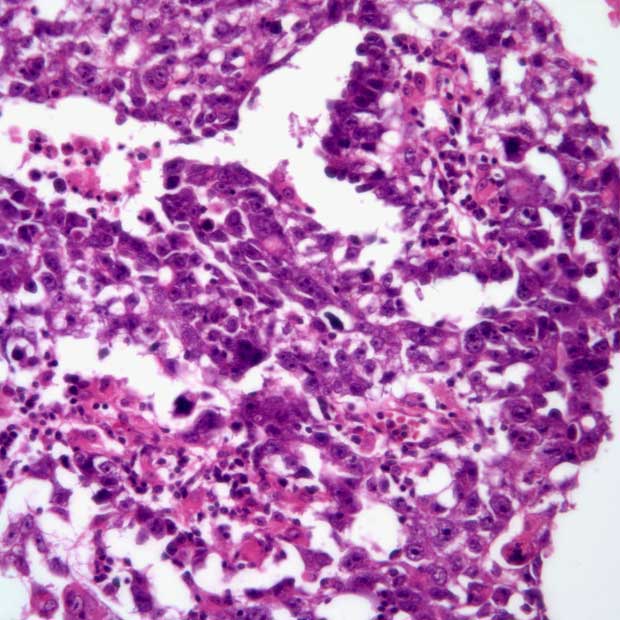
Patients with nonseminomatous testicular cancer who had a complete resection at postchemotherapy retroperitoneal lymph node dissection (RPLND) and less than 10% viable malignant cells appear to experience favorable outcomes without additional treatment, according to findings from a cohort study published in Journal of Clinical Oncology.
Following postchemotherapy RPLND, the 5-year progression-free survival (PFS) rate in patients managed with adjuvant chemotherapy or surveillance, respectively, was 50% vs 53% (P = .31). The corresponding 5-year values in each respective treatment group were 77% vs 70% for cancer-specific survival (CSS; P = .51) and 73% vs 69% for overall survival (OS; P = .54). Investigators reported no differences between surveillance and adjuvant chemotherapy in terms of PFS (HR, 0.72; 95% CI, 0.32-1.6; P = .4), CSS (HR, 0.69; 95% CI, 0.20-2.39; P = .6), or OS (HR, 0.78; 95% CI, 0.25-2.44; P = .7) based on multivariate Cox regression analysis.
Having a good International Germ Cell Cancer Cooperative Group prognostic group (IGCCCG-PG) correlated with improved PFS (HR, 4.05; 95% CI, 1.61-10.2; P = .003), CSS (HR, 9.56; 95% CI, 1.22-74.9; P = .032), and OS (HR, 11.4; 95% CI, 1.49-88.3; P = .019) compared with an intermediate or poor IGCCCG-PG per multivariate Cox regression. Additionally, having less than 10% viable cells in residual masses correlated with longer PFS (HR, 3.22; 95% CI, 1.29-8.0; P = .012) compared with having 10% or more viable cancer cells; conversely, CSS (HR, 2.45; 95% CI, 0.64-9.45; P = .2) and OS (HR, 2.03; 95% CI, 0.61-6.74; P = .2) were reported as being comparable between these groups.
Investigators observed no differences in PFS (P = .95), CSS (P = .11), and OS (P = .11) between patients with good IGCCC-PG only who received surveillance or adjuvant chemotherapy. Among those with intermediate or poor IGCCC-PG, the 5-year PFS rate was 47% for those receiving chemotherapy vs 43% for those receiving surveillance, and the corresponding 10-year rates for each group was 47% vs 17% (P = .049). There were no apparent benefits observed in patients receiving chemotherapy with respect to CSS or OS in the intermediate or poor IGCCC-PG subgroup.
In this retrospective cohort study, investigators collected data on 117 patients who received cisplatin-based frontline chemotherapy and underwent subsequent RPLND from 1990 to 2018 at 13 institutions. Investigators followed patients with surveillance (n = 64) or administered adjuvant chemotherapy to them (n = 53) based on case-by-case discussions with each patient their local clinician.
The study’s primary end points were PFS, CSS, and OS. Investigators stratified patients by IGCCCG-PG risk group classification, Fizazi’s classification, and the use of adjuvant chemotherapy regimens. All patients who were eligible for the study had residual masses of 1 or more centimeters in the largest axial dimension after frontline chemotherapy.
The median patient age was 30 years (interquartile range [IQR], 24-35). Additionally, most patients had a good IGCCCG-PG (32%), received bleomycin plus etoposide and cisplatin in the first-line setting (66%), received 4 cycles of chemotherapy (65%), and completed all cycles of chemotherapy as planned (92%). Most of the study population also had a complete RPLND resection (91%) and negative surgical margins (93%).
Overall, 63 of 117 patients experienced a relapse at a median of 0.4 years (IQR, 0.2-1.4). Of those who relapsed, the most common sites of relapse included the retroperitoneum (53%), the chest (29%), and the liver (22%).
Among patients receiving RPLND at 57 days or fewer, or at more than 57 days following first-line chemotherapy, respectively, the 5-year PFS rates were 52% vs 50% (P = .86), the 5-year CSS rates were 68% vs 79% (P = .25), and the 5-year OS rates were 65% vs 77% (P = .2).
Using Fizazi criteria, investigators classified 10 patients as favorable risk, 32 as intermediate risk, and 18 as poor risk. Those with favorable risk experienced a 5-year PFS, CSS, and OS rate of 100%. Among those with intermediate or poor risk, there were no differences in PFS achieved with adjuvant chemotherapy or surveillance.
Reference
Antonelli L, Ardizzone D, Tachibana I, et al. Risk factors for relapse in nonseminomatous testicular cancer after postchemotherapy retroperitoneal lymph node dissection with viable residual cancer. J Clin Oncol. Published online September 1, 2023. doi:10.1200/JCO.23.00443
Evaluation and Management of Testicular Cancer After Late Relapse
The clinical quandary by Langer et al discusses a contralateral late relapse of the original right nonseminomatous germ cell tumors.