Conservative Approach to CIN 2 a Good Option in Young Women
Conservative management of cervical intraepithelial neoplasia (CIN) grade 2 is an appropriate treatment option for women aged 25 years and younger.
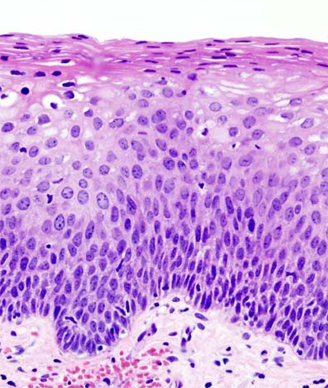
Histopathologic image of a grade 2 cervical intraepithelial neoplasia; source: KGH, Wikimedia Commons
Conservative management of cervical intraepithelial neoplasia (CIN) grade 2 is an appropriate treatment option for women aged 25 years and younger at diagnosis, according to a new retrospective study. The CIN 2 lesions that regress naturally tend to behave similarly to a lower grade lesion.
The age at which women are offered routine cervical screening varies in countries around the world; in New Zealand, where the new study took place, screening begins at age 20, while the US Preventive Services Task Force recommends screening beginning at age 21. “Given that the benefits of screening in this age group may be limited, if screening is to take place, there is a strong obligation to minimize the harms of unnecessary treatment,” wrote study authors led by Tom M. Wilkinson, MBChB, of the University of Otago in Christchurch, New Zealand.
The authors wrote that both grades 2 and 3 CIN tend to be managed using curative treatment, but evidence supporting such therapy in CIN 2 is lacking. “Although CIN 3 has been convincingly shown to carry a high risk of subsequent cancer, CIN 2 is not so obviously precancerous,” the researchers wrote online ahead of print in the American Journal of Obstetrics and Gynecology.
In the new study, a total of 683 women aged younger than 25 years were included: 106 with CIN 2 that spontaneously regressed; 299 with treated CIN 2; and 278 with conservatively managed CIN 1. After a median follow-up period of 4 years, there was no significant difference between the CIN 2 cases that spontaneously regressed and the CIN 1 cases. The adjusted hazard ratio (HR) for development of high-grade abnormalities for those CIN 2 cases compared with CIN 1 after 2 years was 0.92 (95% CI, 0.44-1.94; P = .83).
There was a significantly greater chance of developing high-grade abnormalities in the conservatively managed CIN 2 cases compared with the treated CIN 2 cases, with an HR of 2.97 (95% CI, 1.24-7.09; P = .01). CIN 1 patients also had a higher risk than CIN 2 treated patients, with an HR of 3.23 (95% CI, 1.66-6.29; P = .001).
In total, 18 of 106 CIN 2 spontaneous regression patients eventually developed high-grade abnormalities (17%). In the CIN 1 group, 32 of 278 did so (12%), and 13 of 299 treated CIN 2 patients developed high-grade abnormalities (4%).
Though a larger cohort and prospective design are needed to more fully confirm this approach, the authors wrote that in younger patients this is a reasonable option. “This affirms the value of conservative management of CIN 2 in this group by demonstrating that a large subset of CIN 2 behaves as a low-grade lesion (and hence a case can be made for managing it as one),” they concluded.