Continuous Therapy Best in Newly Diagnosed Multiple Myeloma
Continuous therapy produces drastically better progression-free survival and overall survival outcomes in patients with multiple myeloma. A novel endpoint involving time to second progression is an important tool in evaluating this type of treatment in the future.
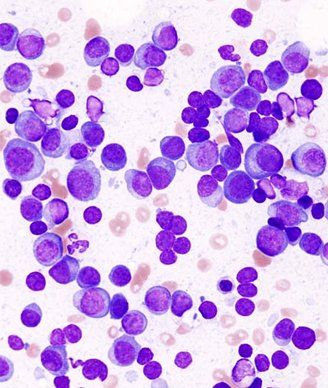
Histopathologic image of multiple myeloma; source: KGH, Wikimedia Commons
Continuous therapy produces drastically better progression-free survival (PFS) and overall survival (OS) outcomes in patients with multiple myeloma. A novel endpoint involving time to second progression is an important tool in evaluating this type of treatment in the future.
Antonio Palumbo, MD, of the University of Torino in Italy, said that in recent years there has been a shift in the treatment paradigm of multiple myeloma, from fixed-duration to continuous treatment. “In myeloma, we always have residual disease,” he said. “When you have residual disease, the need for continuous treatment is essential, because otherwise, the residual disease will grow very quickly.” Dr. Palumbo presented the results (abstract 8515) at the American Society of Clinical Oncology (ASCO) Annual Meeting, held May 30–June 3 in Chicago.
In evaluating fixed-duration vs continuous treatment, though, some trials have used a second PFS outcome, which Dr. Palumbo said is misleading. It measures the time from first progression to second progression, which automatically selects the higher-risk, more resistant patients, which will skew the outcomes. In the new study, which pooled three phase III trials that included treatment with bortezomib or lenalidomide, investigators measured PFS1 (the standard measure of randomization to first progression), as well as PFS2, which measured from randomization to second progression.
The three trials had a total of 1,218 patients, with 604 on continuous therapy and 614 on fixed-duration therapy. After a median follow-up of 52 months, Palumbo said that “the result is honestly quite impressive.” The median PFS1 for continuous therapy was 32 months compared with only 16 months for fixed-duration therapy, with a hazard ratio of 0.47 (95% confidence interval [CI], 0.40–0.56; P < .001). This result was consistent across both bortezomib and lenalidomide, as well as across subgroups, including risk stratification.
Similarly, median PFS2 was 55 months compared with 40 months for fixed-duration therapy, with a hazard ratio of 0.61 (95% CI, 0.50–0.75; P < .001). “The advantage in the first remission is being conserved even in the second remission,” Dr. Palumbo said. Second PFS, meanwhile, only had 687 evaluable patients, and there was no difference between the groups at 15 months median for each (P = .313). There was also an OS benefit with continuous therapy, with a 10-month improvement over fixed-duration therapy (P = .003).
“My conclusion is that PFS2 should be included in all clinical studies comparing fixed-duration therapy and continuous therapy,” he concluded. “Because it is a quick surrogate of survival, and also, probably the evaluation of second PFS only will include a higher proportion of high-risk patients.”
Luciano Costa, MD, PhD, of the Medical University of South Carolina, was the discussant for the session, and agreed that incorporating PFS2 into these trials will be useful. “The benefit of better PFS1 with continuous therapy permeates subsequent lines of therapy, and translates into better PFS2 and, many of us believe, overall survival,” he said. Part of that benefit, he added, is likely due to the fact that relapses are often deadly, and thus patients do not derive benefit from multiple lines of therapy. “Therefore, deeper disease control is likely to benefit OS.”
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.