ctDNA Shows Prognostic Value in Primary Breast Cancer
Findings suggest that patients with breast cancer and consistently negative circulating tumor DNA tests tend to have improved clinical outcomes.
“All told, however, our results suggest that ctDNA testing may add to existing recommendations for symptom assessments, physical examination, and routine breast imaging as a means of monitoring patients with breast cancer after completion of definitive local therapy with or without adjuvant chemotherapy," according to the study authors.
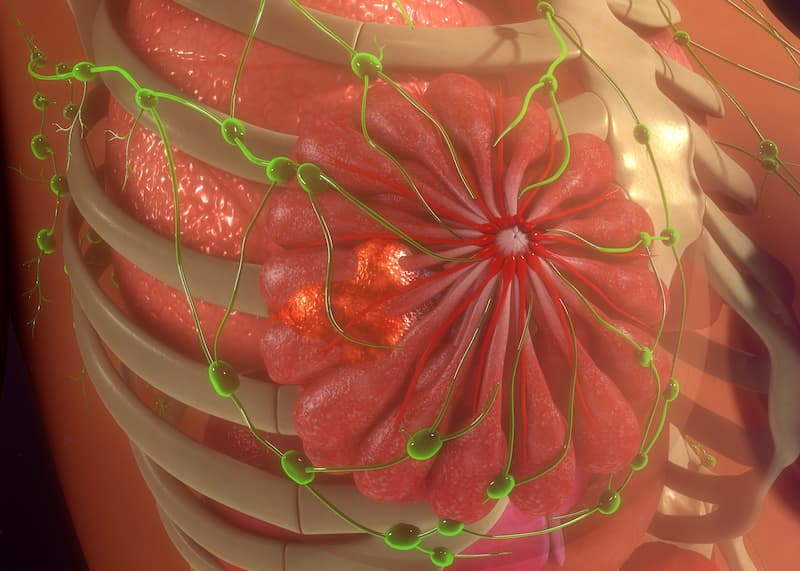
The use of the circulating tumor DNA (ctDNA) assay Signatera demonstrated the ability to predict recurrence in patients with breast cancer, especially among those with triple-negative disease, according to findings from a report published in JCO Precision Oncology.
Among 34 patients who had clinical recurrence at the time of last follow-up, plasma ctDNA was reported in 30, demonstrating a patient-level sensitivity of 88.2%. Additionally, the patient-level sensitivity with the assay was 81.8% for patients with hormone receptor (HR)–positive, HER2-negative disease as well as 100% for those with HR-positive and HER2-positive disease and those with triple-negative breast cancer (TNBC). The 4 patients who relapsed and had no detected plasma ctDNA all had HR-positive, HER2-negative disease.
Worse relapse-free survival (RFS) was highlighted in patients with a positive ctDNA test (HR, 52.98; 95% CI, 18.32-153.20; P <.001); this group also had shorter overall survival (OS) compared with those who had a negative test (HR, 53.69; 95% CI, 7.01-411.49; P <.001). According to multivariate analysis adjusting for clinicopathologic features, ctDNA was still a significant factor that impacted RFS and OS outcomes (P <.001 for each).
“…Serial postoperative ctDNA analysis has strong prognostic value and allows for earlier detection of recurrence than by scans in many patients, while repeated negative tests can provide reassurance to patients,” Jacqueline A. Shaw, PhD, head of the Department of Genetics and Genome Biology, co-director of the Institute for Precision Health, and professor of Translational Cancer Genetics at the University of Leicester, and coauthors wrote. “All told, however, our results suggest that ctDNA testing may add to existing recommendations for symptom assessments, physical examination, and routine breast imaging as a means of monitoring patients with breast cancer after completion of definitive local therapy with or without adjuvant chemotherapy.”
Investigators of the multicenter, prospective Exploratory Breast Lead Interval Study (EBLIS) assessed 156 patients who were 18 years and older with histologically confirmed breast cancer and completed surgery plus adjuvant chemotherapy within 3 years of study entry. Patients underwent follow-up for up to 12 years after completing treatment as well as semiannual blood sampling; investigators collected 1136 plasma samples for ctDNA detection via Signatera assay.
The study’s primary objective was determining a lead interval between the time of detected ctDNA and reported overt metastatic disease. Investigators conducted all personalized, tumor-informed Signatera ctDNA assays in a laboratory with Clinical Laboratory Improvement Amendments certification.
The median follow-up was 77 months (range, 8-140 across the entire population. The study cohort included those with HR-positive, HER2-negative disease (n = 90); HR-positive, HER2-positive disease (n = 35); TNBC (n = 23); and HER2-positive disease (n = 8). Across these different subgroups, anywhere from 12.5% to 43.5% of patients received neoadjuvant chemotherapy, and anywhere from 43.5% to 77% received adjuvant chemotherapy.
In the overall population, metastatic relapse was predicted with a median lead interval between ctDNA detection and relapse of 10.5 months (range, 0-38). Additionally, a median of 8 blood samples (range, 1-11) was collected from patients.
Patients with a relapse had a significantly higher median mean tumor molecules per mL (0.60) compared with those without a relapse (0.12; P = .011). Investigators noted that although this outcome reached statistical significance, the trend occurred based on a small sample of patients without a relapse.
In an analysis of concurrent ctDNA tests and CA15-3 measurements among 100 patients, the Fisher’s exact test highlighted a borderline significant relationship between ctDNA and CA15-3 statuses (P = .053). Additionally, ctDNA appeared to be independent of CA15-3 when predicting RFS and OS based on multivariate analysis, as the former correlated with significantly reduced RFS (HR, 30.89; 94% CI, 10.05-94.99; P <.001) and OS (HR, 35.52; 95% CI, 4.41-285.96; P <.001) compared with the latter.
Reference
Shaw JA, Page K, Wren E, et al. Serial postoperative circulating tumor DNA assessment has strong prognostic value during long-term follow-up in patients with breast cancer. JCO Precis Oncol. 2024;8:e2300456. doi:10.1200/PO.23.00456