Current Guidelines Miss One-Third of RCC Recurrences
If physicians are following the current NCCN and AUA renal cell carcinoma surveillance guidelines, they could be missing as many as one-third of recurrences.
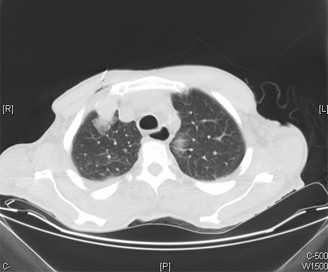
Metastatic renal cell carcinoma; source: Yale Rosen
If physicians are following the current National Comprehensive Cancer Network (NCCN) and American Urological Association (AUA) renal cell carcinoma (RCC) surveillance guidelines, they could be missing as many as one-third of RCC recurrences, results of a study published in the Journal of Clinical Oncology showed.
“In fact, we found that 31.8% and 33.1% of all primary recurrences would have been missed by the 2014 NCCN and AUA guidelines, respectively, and that 64.1% of primary recurrences would have been missed if following the 2013 NCCN guidelines,” wrote researchers led by Suzanne B. Stewart, MD, of Mayo Clinic, Rochester, Minn.
However, the analysis by Stewart and colleagues also found that if surveillance of these patients were extended to capture 95% of recurrences, patients would require surveillance for 14 years or longer and Medicare surveillance costs would greatly increase.
In an editorial that accompanied that article, Angela B. Smith, MD, and Matthew I. Milowsky, MD, of the University of North Carolina Lineberger Comprehensive Cancer Center, called the results striking, but added a few additional points to help put the results in perspective.
First, they noted that the results were taken from a single center making it difficult to generalize more widely. Next, because the researchers found higher recurrence rates among low-risk radical nephrectomy patients, physicians may lack an accurate system for characterizing low- and high-risk RCC.
“Gaining a better understanding of tumor biology may improve risk stratification and translate to a surveillance regimen that more accurately captures meaningful recurrences (ie, those that require treatment, affect survival outcomes, or diminish quality of life),” Smith and Milowsky wrote. However they added that “arguing for extending surveillance without understanding its role on outcomes is the definition of putting the cart before the horse.”
In the study, Stewart and colleagues evaluated 3,651 patients with RCC who underwent surgery between 1970 and 2008. Patients were grouped as AUA low risk after partial (LR-partial) or radical nephrectomy (LR-radical), or as moderate/high risk. Using current guidelines, the researchers calculated how many recurrences could have been detected.
At a median follow-up of 9 years, 29.8% of the patients had an RCC recurrence. Using the 2013 NCCN guidelines, only 35.9% of these recurrences would have been detected; 68.2% could have been detected using 2014 NCCN guidelines, and 66.9% using current AUA guidelines.
According to the researchers, all three surveillance guidelines missed the greatest number of recurrences in the abdomen and among pT1, Nx-0 patients.
Data indicated that in order to fully capture 95% of the RCC recurrences that occurred, patients with LR-partial disease would have to undergo surveillance for 15 years; those with LR-radical disease, 21 years; and those with moderate/high-risk disease, 14 years.
In addition, although Medicare surveillance costs for a patient with LR-partial disease is between $1,000 and $2,000 using current guidelines, if surveillance were extended to capture 95% of recurrences, the Medicate surveillance costs would be greater than $9,000.
“Thus, further research remains necessary to identify an optimal surveillance approach that balances patient benefit and health care costs,” the researchers wrote.