Cyclophosphamide Effective Substitute for Ifosfamide in Ewing Sarcoma
A new study found that clinicians may be able to safely substitute cyclophosphamide for ifosfamide in the consolidation treatment of standard-risk Ewing sarcoma.
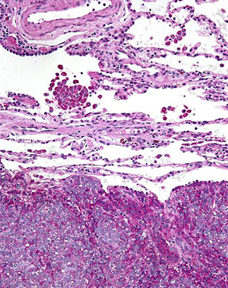
High magnification micrograph of Ewing sarcoma in lung; PAS stain; source: Nephron, Wikimedia Commons
Clinicians may be able to safely substitute cyclophosphamide for ifosfamide in the consolidation treatment of standard-risk Ewing sarcoma, according to the results of the Euro-EWING99-R1 trial published in the Journal of Clinical Oncology.
“These results could lead to decreased burden of treatment and toxicity in Ewing sarcoma patients,” Marie-Cécile Le Deley, MD, PhD, of Gustave Roussy Institute, told Cancer Network, adding that the ongoing comparative evaluation of patients treated with vincristine, dactinomycin, ifosfamide (VAI) vs vincristine, dactinomycin, cyclophosphamide (VAC) in terms of late effects on kidney function and fertility is crucial to decisions regarding future patients.
According to Le Deley, in the early days of Ewing sarcoma chemotherapy, cyclophosphamide was given in combination with other agents. In the late 1980s, in attempts to improve outcome, cyclophosphamide was progressively replaced by ifosfamide, in single-arm studies, as it had the advantage of less myelotoxicity at higher dosage. However, chronic renal tubular damage related to the cumulative dose of ifosfamide along with uncertainty of greater efficacy of ifosfamide vs cyclophosphamide led to questioning ifosfamide as a standard backbone chemotherapy in Ewing sarcoma. Although randomized trials compared ifosfamide-based to cyclophosphamide-based chemotherapy in sarcomas, they were very rare and had limited sample size.
The EURO Ewing 99 trial is a pan-European collaboration between pediatric and adult oncologists. In it, researchers sought to assess the value of ifosfamide compared to cyclophosphamide in the treatment of Ewing sarcoma.
Le Deley and colleagues enrolled 856 patients with standard-risk Ewing sarcoma between February 2000 and March 2010. Patients were given six courses of vincristine, ifosfamide, doxorubicin, and etoposide plus one cycle of VAI and were then allocated to treatment with seven VAC courses or VAI courses. The median follow-up was 5.9 years.
Overall, 86% of patients in the study were alive at 3 years, and 77% were free of relapse. The 3-year event-free survival was similar between the two treatments arms (75.4% for VAI vs 78.2% for VAC).
As expected, renal tubular function impairment was 50% lower in patients assigned VAC compared with VAI (16% vs 31%; P < .001). Patients in the VAC had an increased likelihood of hematologic toxicity compared with the VAI arm (45% vs 35%).
“Some uncertainty surrounding relative efficacy of cyclophosphamide (VAC group) compared to ifosfamide (VAI group) remains at this stage,” Le Deley said. “In particular, we observed a trend toward ifosfamide for male patients, but this finding warrants further investigation. More important, the overall balance in terms of long-term toxicity still needs to be addressed.”
William H. Meyer, MD, of the University of Oklahoma Health Sciences Center, and Holcombe E. Grier, MD, of Dana-Farber/Boston Children’s Cancer and Blood Disorder Center, wrote an editorial accompanying the research.
“These study results provide reasonable assurance that, after intensive induction therapy with vincristine, ifosfamide, doxorubicin, and etoposide, VAC and VAI consolidation treatment for standard-risk Ewing sarcoma will provide indistinguishable survival outcomes,” they wrote. “The challenge for our present and future investigations is to ensure that questions we ask now can be answered in a reasonable time frame and will be relevant once study accrual is complete and data are analyzed.”
Sarcoma Awareness Month 2023 with Brian Van Tine, MD, PhD
August 1st 2023Brian Van Tine, MD, PhD, speaks about several agents and combination regimens that are currently under investigation in the sarcoma space, and potential next steps in research including immunotherapies and vaccine-based treatments.