Deep Molecular Response to TKI Therapy Predicts Better Survival in CML
A deep molecular response to imatinib, achieved by most chronic myeloid leukemia patients who receive the drug, is predictive of better overall survival, according to a new study.
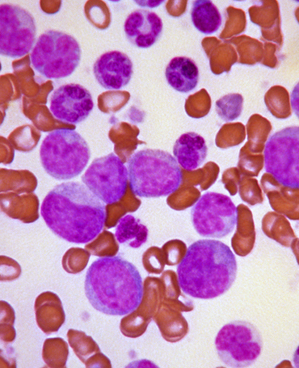
Peripheral blood smear revealing the histopathologic features indicative of a blast crisis in a case of CML
A deep molecular response to the tyrosine kinase inhibitor (TKI) imatinib, achieved by most chronic myeloid leukemia (CML) patients who receive the drug, is predictive of better overall survival, according to a new study. The response predicted outcomes better than complete cytogenetic response (CCR).
The new study, led by Rudiger Hehlmann III, MD, of Universitat Heidelberg in Germany, was published in December in the Journal of Clinical Oncology. The study cohort included 1,551 randomized patients in the CML-Study IV; 1,524 of those were evaluable and included in the final analysis. A deep molecular response was defined as at least a 4.5 log reduction in BCR-ABL on the international scale (MR4.5).
The cumulative incidence of MR4.5 after 9 years was 70%, with a median of 4.9 years elapsed until MR4.5 was achieved. The deeper response was achieved more quickly with optimized higher dose imatinib of 800 mg/day over the more standard 400 mg/day (48 months vs 62 months; P = .016).
The 5-year overall survival rate was 90% in the full cohort, and 5-year progression-free survival was 87.5%; 8-year overall survival was 86%. Regardless of which imatinib dose was used, achieving MR4.5 at 4 years predicted higher survival probability than CCR (8-year overall survival, 92% vs 83%; P = .047). Both higher dose of imatinib and early major molecular remission were independent predictors of MR4.5.
"Very deep remissions can be achieved with imatinib in the majority of CML patients," Dr. Hehlmann told Reuters Health. He added that this suggests that “deep molecular response is a precondition for treatment discontinuation."
A number of studies have recently found that discontinuation of imatinib is feasible in patients who respond well to the drug. One phase II study in Europe found that some patients did not relapse after discontinuation, and responses even persisted without the drug. Another study found 18 of 40 patients (45%) who discontinued imatinib had no evidence of relapse after a median of 42 months; in that trial, slower achievement of a more complete response was correlated with higher relapse risk.
In the new study, the investigators concluded that MR4.5 should be considered a new predictor of long-term outcome, and it may “provide an improved therapeutic basis for treatment discontinuation in CML.” The interest in discontinuation of treatment is directly related to the impressive success of TKIs in CML; because the drugs have raised the average survival duration dramatically in many patients, the need to keep taking them for decades has become an issue of cost, compliance, and other factors.