Dendritic Cell Vaccine Improved PFS, Not OS in Glioblastoma
A phase II trial evaluating the use of a dendritic cell vaccine, ICT-107, has shown that the immunotherapy had a positive effect on progression-free survival in patients with glioblastoma.
ICT-107 slowed disease progression in glioblastoma patients.
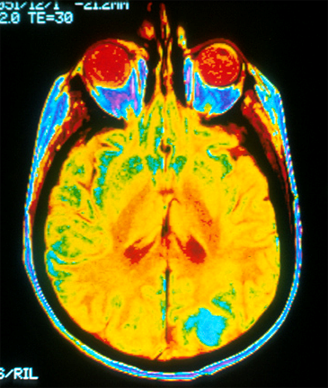
CHICAGO-A phase II trial evaluating the use of a dendritic cell vaccine, ICT-107, has shown that the immunotherapy had a positive effect on progression-free survival in patients with glioblastoma. However, the trial failed to meet its primary endpoint of overall survival.
“This data is not mature and perhaps with more time and more events this improvement in progression-free survival could translate to overall survival,” said investigator Patrick Y. Wen, MD, of Dana-Farber Cancer Institute, who presented the results Sunday at the 2014 American Society of Clinical Oncology (ASCO) Annual Meeting (abstract #2005).
The study included patients with HLA-A1–positive or HLA-A2–positive glioblastoma; 124 patients were randomly assigned 2:1 to treatment with the ICT-107 vaccine or to the control arm. The regimen consisted of four induction doses of the vaccine after chemoradiation, and then maintenance doses until disease progression. ICT-107 is an autologous six-antigen dendritic cell vaccine.
The trial failed to meet its overall survival primary endpoint. Results analyzed in April 2014 indicted that the median overall survival was not statistically different for patients receiving the ICT-107 vaccine and those in the control arm in the intent-to-treat population (median OS 18.3 vs 16.7 months) or the per-protocol population (median OS 18.6 vs 16.7 months). Wen noted that the data show a numeric improvement in overall survival with the study treatment, but that it did not reach statistical significance.
However, the researchers did observe differences in progression-free survival. In the intent-to-treat population the median progression-free survival was 11.2 months for the ICT-107 patients compared with 9 months for control. In the per-protocol analysis, median progression-free survival was 11.4 months compared with 9 months.
Looking at overall survival in patients with unmethylated MGMT promotor status and HLA-A2, the median overall survival was 15.8 months for patients receiving the vaccine compared with 11.8 months for patients in the control arm, a nonsignificant difference.
The vaccine was found to be strong in the methylated MGMT and HLA-A2–positive subgroups. In the per-protocol analysis, the median progression-free survival for patients assigned ICT-107 was 24.1 months compared with 8.5 months for patients in the control arm, a benefit of more than 15 months.
A quality-of-life analysis showed that patients receiving the ICT-107 vaccine had greater performance capacity, as measured by Karnofsky Performance Status, than patients in the control arm and tended to be placed on steroids later in the course of treatment.
Overall the vaccine was well tolerated. Of the grade 4 or higher toxicities seen on the trial, none of them were thought to be treatment related, Wen said.
“ICT-107 is strongest in the HLA-A2 subgroup clinically, immunologically, and with regard to antigen expression,” Wen said. “This activity is observed in both the MGMT methylated and unmethylated subgroups.”
In addition, vaccine potency as measured by HLA-DR expression and IL-2 secretion was predictive of overall survival.
Based on these results, Wen said that this trial should advance to a phase III trial.