Denosumab Biosimilars Available in the US for Bone Mets, Multiple Myeloma
The 2 denosumab biosimilars previously received FDA approval for select patients with multiple myeloma, solid tumor bone metastases, and osteoporosis.
Approval was supported by results from a double-blind, active-controlled, phase 3 study, which compared efficacy outcomes, as well as pharmacokinetics, pharmacodynamics, and safety of CT-P41 vs Prolia in postmenopausal women with osteoporosis.
Two indications of denosumab-bmwo (CT-P41; Stoboclo, Osenvelt), referencing 2 other denosumab indications (Prolia, Xgeva), have become commercially available in the US as a treatment for select patients with osteoporosis, multiple myeloma, and solid tumors with bone metastases, according to a news release from the developer, Celltrion USA.1
Both indications of denosumab-bmwo were previously approved by the FDA in March 2025.2 Approval was supported by results from a double-blind, active-controlled, phase 3 study (NCT04757376), which compared efficacy outcomes, as well as pharmacokinetics, pharmacodynamics, and safety of CT-P41 vs Prolia in postmenopausal women with osteoporosis.3 Therein, patients experienced comparable outcomes with both agents.
"We are pleased to have achieved a global settlement with Amgen regarding our denosumab biosimilars," Thomas Nusbickel, chief commercial officer at Celltrion USA, said in the news release.1 "We are proud to introduce our denosumab biosimilars to the US market, offering patients and healthcare professionals a valuable alternative treatment option. Building on our strong heritage in biosimilars, Celltrion remains committed to being a trusted partner for both patients and physicians, while contributing to the overall sustainability of healthcare systems."
Both Stoboclo and Osenvelt were approved by the European Medicines Agency (EMA) in February 2025.
Stoboclo
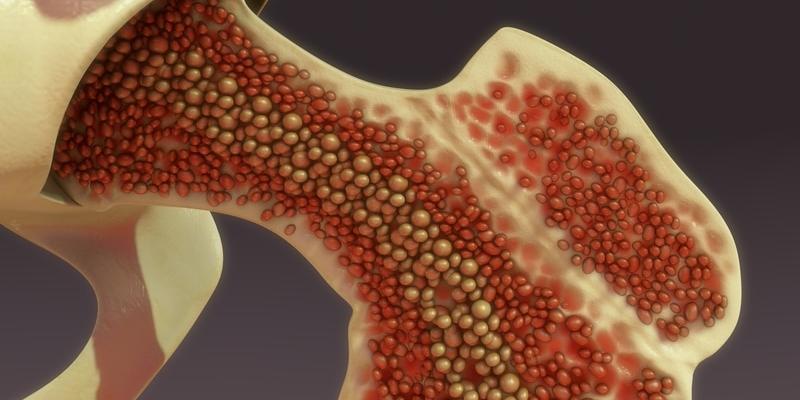
Stoboclo is a RANKL inhibitor referencing Prolia and is approved in the US at a dose of 60 mg/mL for the treatment of: postmenopausal women with osteoporosis; men with osteoporosis or those receiving androgen deprivation therapy for nonmetastatic prostate cancer; glucocorticoid-induced osteoporosis; and women receiving an adjuvant aromatase inhibitor for breast cancer. All indications include having a high fracture risk.
In a 3-year, multinational study of 7808 postmenopausal women from 60 to 91 years, 3876 received placebo and 3886 received 60 mg of subcutaneous denosumab every 6 months.4 Efficacy data revealed that the incidence of all-cause mortality in the respective arms was 2.3% vs 1.8%, respectively. Additionally, 24.2% vs 25.0% experienced nonfatal serious adverse events (AEs), and 2.1% vs 2.4% of each respective group withdrew from study participation due to AEs. The most common AEs in the denosumab and placebo cohorts included back pain (34.7% vs 34.6%), pain in extremity (11.7% vs 11.1%), musculoskeletal pain (7.6% vs 7.5%), hypercholesterolemia (7.2% vs 6.1%), cystitis (5.9% vs 5.8%), and vertigo (5.0% vs 4.8%).
Furthermore, the safety of the Stoboclo was assessed in a 1-year primary analysis of a 2-year randomized study, wherein 795 patients undergoing treatment for glucocorticoid-induced osteoporosis were randomly assigned 1:1 to receive an active control consisting of 5 mg of oral daily bisphosphonate (n = 384) or 60 mg of subcutaneous denosumab every 6 months (n = 394). The incidence of all-cause mortality was 0.5% with active control and 1.5% with denosumab. The incidence of serious AEs was 17% vs 16% in each respective group, and 3.6% vs 3.8% withdrew from the study due to AEs.
Additionally, the safety of denosumab was assessed in a 3-year randomized study, wherein 1468 patients with nonmetastatic prostate cancer ages 48 to 87 years old undergoing treatment for bone loss related to androgen deprivation therapy were randomly assigned 1:1 to receive placebo (n = 725) or 60 mg of subcutaneous denosumab every 6 months (n = 731). The incidence of serious AEs was 30.6% vs 34.6% in each respective group, and 6.1% vs 7.0% withdrew from the study due to AEs.
In a 2-year randomized controlled trial, the safety of denosumab in the treatment of bone loss in 252 women ages 35 to 84 years old with nonmetastatic breast cancer receiving aromatase inhibitor therapy received placebo (n = 120) or 60 mg of subcutaneous denosumab every 6 months (n = 129). The incidence of serious AEs was 9.2% vs 14.7% in the respective arms, with 4.2% and 0.8% discontinuing therapy due to AEs.
Osenvelt
Another RANKL inhibitor, Osenvelt, a therapeutic equivalent to Xgeva, is approved in the US as a 70 mg/mL injection for the prevention of skeletal-related events in patients with solid tumor-originating bone metastases, as well as multiple myeloma. It is also approved for the treatment of adults and skeletally mature adolescents with unresectable giant cell tumor of bone, as well as for the treatment of bisphosphonate-refractory hypercalcemia malignancies.
Osenvelt was investigated across 3 studies: study 20050136 (NCT00321464) evaluated the treatment in patients with advanced breast cancer and bone metastasis; study 20050244 (NCT00330759) evaluated the treatment in patients with solid tumors, other than breast and castration-resistant prostate cancer, with bone metastasis and multiple myeloma; and study 20050103 (NCT00321620) evaluated the treatment in patients with castration-resistant prostate cancer and bone metastasis.5
The most common adverse reactions were fatigue or asthenia, nausea, and hypophosphatemia in patients with bone metastases from solid tumors. At least 10% of those with multiple myeloma experienced diarrhea, nausea, back pain, anemia, peripheral edema, thrombocytopenia, rash, headache, and upper respiratory tract infection. Additionally, arthralgia, nausea, fatigue, back pain, headache, and pain in extremity occurred in at least 10% of patients with giant cell bone tumor. Furthermore, nausea, decreased appetite, peripheral edema, headache, dyspnea, anemia, constipation, and diarrhea were observed in 20% or more of patients with hypercalcemia of malignancy.
References
- Celltrion USA announces U.S. launch of denosumab biosimilars, STOBOCLO® and OSENVELT® (denosumab-bmwo). News release. Celltrion USA. July 7, 2025. Accessed July 10, 2025. https://tinyurl.com/er2pfvzn
- Celltrion receives U.S. FDA approval for STOBOCLO® (denosumab-bmwo) and OSENVELT® (denosumab-bmwo) biosimilars referencing PROLIA¬Æ and XGEVA¬Æ. News release. Celltrion. March 4, 2025. Accessed July 10, 2025. https://tinyurl.com/ahnwrx57
- A phase 3 study to compare between CT-P41 and US-licensed Prolia in postmenopausal women with osteoporosis. ClinicalTrials.gov. Updated June 14, 2024. Accessed July 10, 2025. https://tinyurl.com/mumw3my6
- Prescribing information. STOBOCLO U.S. prescribing information. FDA. 2025. Accessed July 10, 2025. https://tinyurl.com/3axp9x9a
- Prescribing Information. OSENVELT U.S. prescribing information. FDA. 2025. Accessed July 10, 2025. https://tinyurl.com/2h9x6dce
How Supportive Care Methods Can Improve Oncology Outcomes
Experts discussed supportive care and why it should be integrated into standard oncology care.