Delirium is frequently encountered when caring for cancer patients, from initial diagnosis to the advanced stages of the disease; however, it is often missed. Oncologists need to be familiar with the various defining features of the condition, and should be able to identify common underlying causes. We present a systematic approach to the workup, as well as pharmacologic and nonpharmacologic approaches to management. We discuss the common practice of treatment with neuroleptics, as well as recent controversy surrounding their use.
Introduction
While written accounts of delirium date back centuries, these older descriptions often depict the condition in a fatalistic light-as the harbinger of imminent death. Modern medicine allows for a more nuanced view of the diagnosis, treatment, and overall course of delirium.
Although ubiquitous across all medical specialties, delirium plays a prominent role in oncology. Patients are exposed to multiple modalities of treatment, such as chemotherapy and immunotherapy, surgery, and radiation, all of which can influence cognition in a fluctuating pattern. Chronic conditions often seen in cancer patients, such as pain, nausea, and anxiety, are also treated with potentially deliriogenic agents. While delirium is typically considered a condition of the acute medical setting, cancer patients may report it in the outpatient setting as well.[1] Incidence estimates range from 43% in the general cancer population to 85% in patients in the terminal stages of their illness,[2] making delirium one of the most common cancer comorbidities, although it often goes unrecognized.
Diagnosis
The commonly accepted criteria for delirium, found in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), have remained relatively stable over time. These include an alteration in attention and awareness (Criterion A) that occurs within a span of hours to days, fluctuating in severity several times in the course of a day (Criterion B). There are also disturbances in other aspects of the patient’s mental state, which can include, but are not limited to, aphasia, amnesia, disorientation, visuospatial changes, and hallucinations (Criterion C). Finally, there should be clinical evidence that this presentation is directly related to some physiologic insult, including medication or withdrawal syndromes, as opposed to being due to a preexisting neurocognitive condition (Criteria D and E, respectively). In a phenomenological study of 100 palliative care patients with delirium,[3] the most common disturbance was in attention (97%), followed by long- and short-term memory impairment (89% and 88%). Less common were disturbances in orientation (76%) or perception (50%). Thus, if physicians rely on the presence of hallucinations or disorientation, they can miss potentially treatable cases.
Of note, the DSM-5 criteria do not mention disruption in sleep cycle or changes in motor activity-frequent hallmarks of delirium-although these are described in the International Classification of Diseases, Tenth Revision (ICD-10) criteria. Furthermore, the DSM-5 criteria lack specifiers, such as the hyperactive subtype (characterized by disinhibition and often violent activity), the hypoactive subtype (a withdrawn, almost catatonic, state), and the mixed subtype. Despite these limitations, the DSM-5 criteria remain useful for their high inter-rater reliability.[4]
Commonly used instruments for delirium screening include the 10-question Confusion Assessment Method (CAM), which is notable for its versatility: the CAM is available in a shortened four-item algorithm; there is a family-administered version, referred to as FAM-CAM, which makes it possible for families to screen for delirium; and finally, CAM-ICU has been specifically developed for delirium screening of patients in intensive care units who are unable to speak. The Memorial Delirium Assessment Scale (MDAS) is a rating instrument commonly used to monitor the progression of delirium, but it can also be employed for screening.[5] The Short Blessed Test is a sensitive series of four weighted questions that can assess attention and orientation quickly and in multiple settings, although it is not specific enough to rule out other neurocognitive disorders.[6]
In addition to understanding the criteria for a diagnosis of delirium, oncologists must maintain strong clinical vigilance. In one study that followed 771 cancer patients referred to palliative care for consultation, 33% met criteria for delirium when seen by a consultant, but the majority of these (61%) had not been diagnosed by the referring team.[1] Similarly, in a case series of 60 cancer patients seen by consulting psychiatrists and ultimately diagnosed with delirium, 37% of the diagnoses had initially been missed.[7]
Diagnosis of delirium in the cancer population can be challenging for several reasons. Cancer-related cognitive impairment is a common complaint among patients.[8] It can be difficult to distinguish delirium from the more chronic alterations in attention, executive function, and energy associated both with cancer treatment and with the disease itself. Accordingly, it is useful to obtain collateral information from caretakers and family members to provide a clear chronology for events such as losing items in the house, getting lost, having difficulty with language and directions, displaying alterations in sleep, etc. Particular focus should be put on acuity and fluctuation in these symptoms, as well as on possible precipitating factors (eg, medications, constipation/urinary retention, abrupt changes in environment).
Mood and anxiety symptoms are also common comorbidities in cancer patients and can obfuscate the diagnosis of delirium. Major depressive disorder itself can impact cognition and concentration, particularly when it presents in its most severe form. However, even in patients with major depressive disorder, high clinical suspicion should be maintained for delirium, particularly in those without any significant psychiatric history prior to their cancer diagnosis. Psychiatrists are consulted frequently for depression when a patient appears to lose interest in his or her self-care or treatment, but they often find that the patient’s withdrawal is secondary to a hypoactive delirium.[9-11] Distinguishing between depression and hypoactive delirium is a particular challenge with older cancer patients.[12]
Treatment and Prevention
Preventing delirium
All physicians working in the acute setting should familiarize themselves with the National Institute for Health and Care Excellence (NICE) guidelines for delirium prevention, which offer simple, economic interventions that can limit potentially costly and catastrophic events.[13] Preventive measures have generally been focused on the most vulnerable: elderly, postoperative patients. Korc-Grodzicki et al demonstrated that a preoperative geriatric assessment in patients with solid tumors can be used to identify risk factors for the development of delirium that results in a longer hospital course and discharge to a rehabilitation facility.[14]
Treatment begins and ends with treating the physiologic insult
Attempting to manage the symptoms of delirium without addressing the underlying physiologic cause is akin to pouring water onto a fire being fed by an open gas line. While it can be contained by symptom management, the delirium will only resolve with the treatment of underlying pathology.
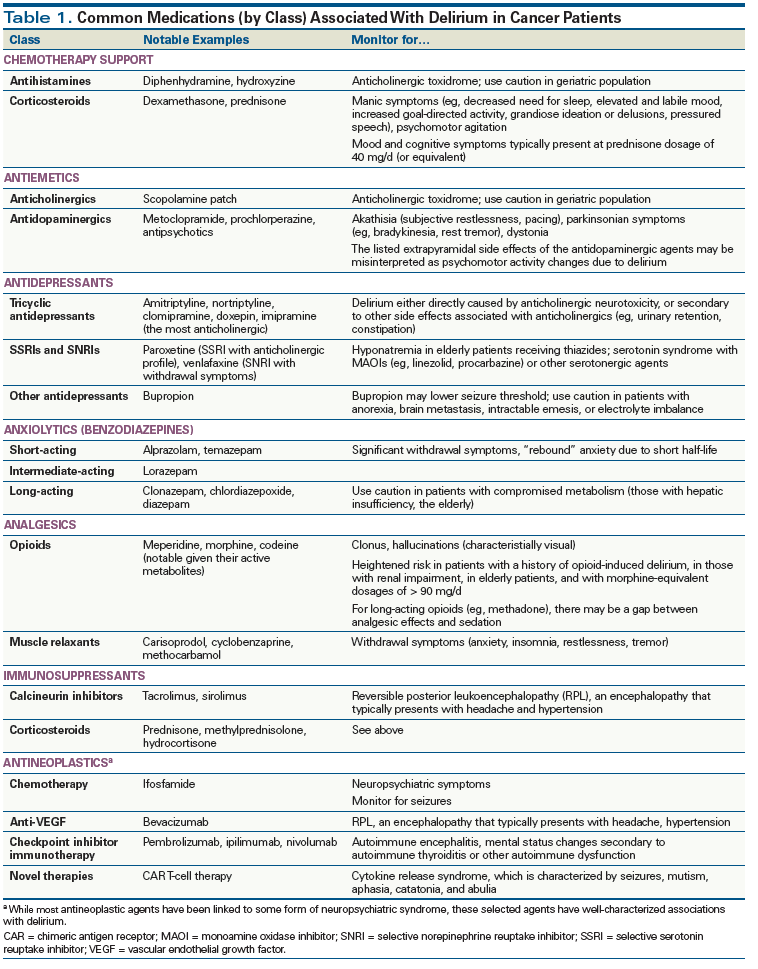
The workup of delirium in the general population has been discussed extensively in the medical literature and won’t be repeated here. It is important to remember that cancer patients are not any more immune to conditions such as alcohol dependence or illicit substance abuse than others in the general population; it is thus important to keep these factors in the differential diagnosis. However, the situation of cancer patients also has an inherent complexity, resulting from the interplay of their illness, comorbidities, and often toxic treatments, and leading to multifactorial etiologies for delirium. Therefore, the first step in the workup should always be a detailed history, with close attention paid to any changes in medication. A complete list of deliriogenic medications is outside the scope of this article, but there are several that are frequently encountered in cancer care; these are listed in Table 1.
KEY POINTS
- Delirium remains one of the most prevalent cancer comorbidities, yet it is often undetected.
- Taking a systematic approach to identifying and treating the physiologic cause of delirium, while remaining mindful of the overall goals of care, can shorten the course of delirium and alleviate patient distress.
- Judicious and thoughtful use of antipsychotics remains the gold standard for treatment of delirium-associated distress and behavioral disturbances in patients who have not responded sufficiently to nonpharmacologic measures.
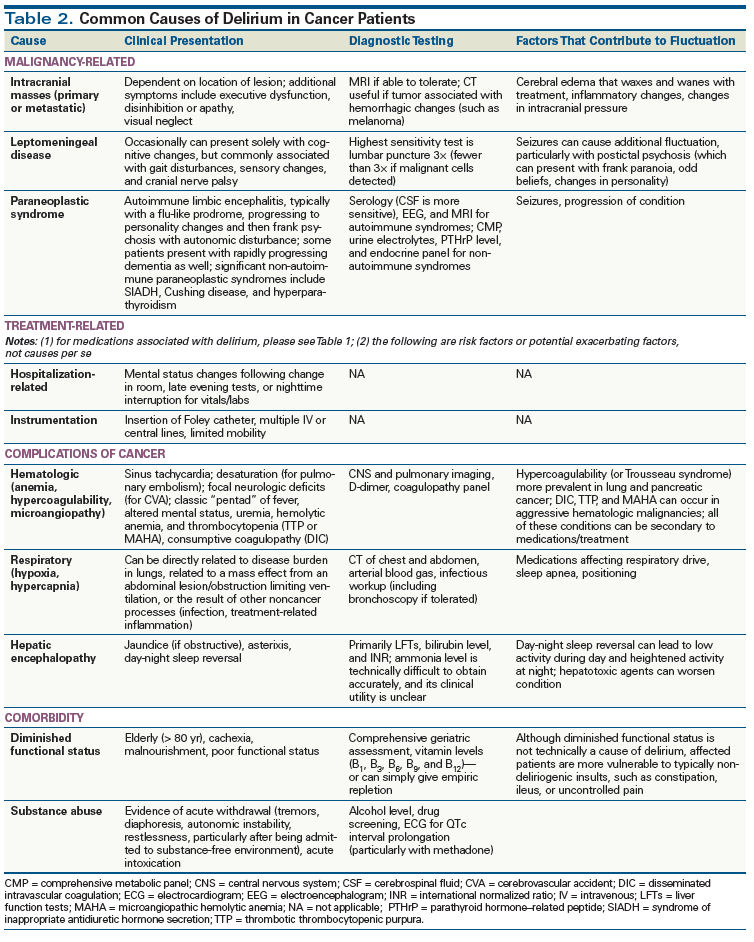
The laboratory and imaging workup for delirium in cancer patients follows the same general principles as the workup for delirium associated with other medical conditions. However, the medical complexity of cancer patients warrants a categorical approach: causes can arise from the cancer itself, treatment-related side effects, complications, and comorbidities. As the illness progresses, the cause of delirium becomes multifactorial, and more difficult to tease apart.
Clinicians should always be mindful of the overall goals of care, and should engage both the patient and his or her family to ensure that evaluation and treatment are in line with personal beliefs, and that the rationale for medical decisions is clearly communicated. While identifying and treating the physiologic insult is usually the principal goal, there are cases where otherwise appropriate tests or treatments might be contraindicated; for example, even seemingly benign interventions, such as head imaging, may be disorienting and traumatizing without significant clinical yield.
Cancer-related causes. Delirium directly caused by malignancy varies in presentation, depending on site and tumor type (Table 2). For example, central nervous system (CNS) cancer, either primary or metastatic, can cause fluctuation in mental status secondary to waxing and waning edema or inflammation. Even when CNS imaging is negative, patients who present with signs of delirium and exhibit an abrupt change in gait or motor disturbances, cranial nerve palsies, or sensory changes should have at least three lumbar punctures to definitively rule out leptomeningeal disease. There should be a low threshold for use of electroencephalography (EEG) to rule out nonconvulsive status epilepticus, as well as postictal changes, the latter of which can present with frank paranoia, odd religious beliefs, and perceptual disturbances, mimicking a primary psychotic disorder.
Paraneoplastic syndromes, especially the autoimmune encephalitides, pose a particular challenge to clinicians. In certain patients, autoantibodies that form against tumor antigens target structures in the host limbic system. This limbic encephalitis gives rise to neuropsychiatric symptoms consistent with classic delirium. Given the rarity of paraneoplastic syndromes, it would not be feasible or economically responsible to screen for them in all cases of altered mental status. However, the reasons to forgo screening for these syndromes need to be balanced against the fact that they are potentially reversible conditions. The most commonly implicated tumors include small-cell lung cancer, ovarian teratoma, thymoma, and testicular cancer.[15] As autoimmune paraneoplastic syndromes gain more recognition, there have been increased reports of them in patients with non–small-cell lung cancer and breast cancer, although given the prevalence of these malignancies, the findings could be due to selection bias.[16] The diagnostic gold standard for paraneoplastic syndromes involves serum or cerebrospinal fluid serology; however, before ordering serologies, there should be some suspicion based on a relatively rapid progression of neuropsychiatric symptoms, with subacute onset, evidence of inflammation on MRI (eg, lesions in the limbic system on T2-weighted imaging), evidence of temporal lobe epileptogenic activity on EEG, and the exclusion of other more common etiologies.[17]
Other extracranial mechanisms of delirium include hepatic encephalopathy if the cancer has extended to the liver; although there is some debate about the utility of checking ammonia levels, given the unclear correlation between these levels and mental status changes, as well as technical challenges, providers should check for asterixis and day-night sleep reversal (with the caveat that these are nonspecific findings).
Treatment-related causes. Cancer treatment typically involves the use of toxic agents, accompanied by additional palliative medications to manage the side effects of treatment. Both types of agents necessitate close monitoring for delirium. Table 1 provides some common agents to be aware of, but this list is by no means comprehensive. Clinicians should take stock not only of what the patient is currently taking, but also of any medications recently discontinued, including abrupt taper of corticosteroids (which can result in adrenal insufficiency and electrolyte imbalance) and of psychotropics associated with withdrawal syndromes.
Treatment can also involve otherwise benign nonpharmacologic measures that increase the risk of delirium. Abrupt changes in hospital rooms, diagnostic testing and procedures in the late evening, as well as restrictions in movement required for treatment, can all lead to delirium, particularly in vulnerable populations such as the elderly or the cognitively impaired.
Cancer complications. Several hematologic sequelae of cancer can lead to delirium. Lung and pancreatic disease have been linked to higher rates of cancer-associated hypercoagulability, also known as Trousseau syndrome. This can lead to cerebral vascular accidents[18] or large pulmonary emboli, which in turn can result in abrupt changes in behavior. Aggressive hematologic malignancies often give rise to disseminated intravascular coagulation or thrombotic thrombocytopenic purpura, both with associated changes in mentation.
While delirium arising from malnutrition is not unique to cancer, oncology patients are at increased risk for nutritional deficiency and malabsorption. Thiamine deficiency and cachexia, followed by rapid repletion of sugar and subsequent Wernicke encephalopathy, is now being recognized outside of alcohol use disorder with increased frequency.[19,20] Given the availability and minimal adverse effects, we favor empiric repletion of thiamine (500 mg intravenously TID for 3 days, followed by 100 mg daily) in any patient in whom Wernicke encephalopathy is suspected.
Electrolyte disturbances are common, due to either malnourishment or gastrointestinal/urinary loss. Syndrome of inappropriate antidiuretic hormone secretion (SIADH) should always be in the differential when fluctuating mental status associated with hyponatremia is present; SIADH may be either a paraneoplastic syndrome or a result of medication.
Finally, poor cerebral perfusion is one of the most challenging causes of delirium to manage. It can be related to hypoxia due to diminished lung diffusion, pulmonary edema (malignant or otherwise), or hypercapnia from compromised ventilation. Abrupt onset of anemia will have similar effects, depriving the brain of essential gas exchange.
Comorbidities. While causes of delirium outside of cancer are beyond the scope of this feature, physicians should be mindful that cancer is not protective against substance abuse. Intoxication and withdrawal from alcohol, benzodiazepines, and barbiturates should always be in the differential diagnosis of delayed change in mental status.
Treatment
Use of psychotropics
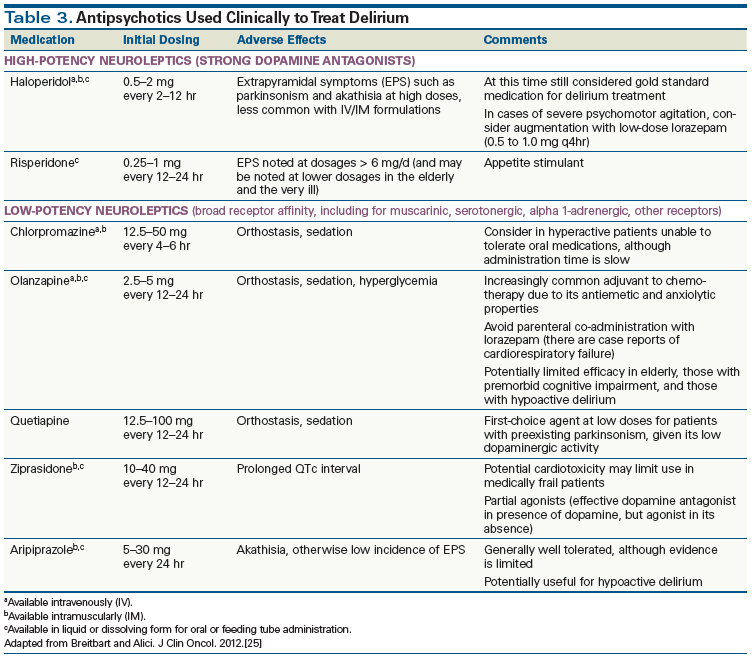
Although neuroleptics have been the subject of controversy, common clinical practice now favors their use-and the avoidance of benzodiazepines. While antipsychotics are often categorized based on when they were introduced, with older medications referred to as “first-generation” or “typical” antipsychotics, the more meaningful distinction involves affinity and effect on the dopamine-2 (D2) receptor. Higher-affinity, or high-potency, agents have a more targeted antagonism of dopamine, an excess of which is believed to account for the altered sensorium in delirium. Agents with a greater effect on dopamine carry a higher risk of extrapyramidal symptoms, and should be avoided in patients at risk for parkinsonism. Agents said to have lower affinity or potency will block several other neuroreceptors in a nonspecific pattern before saturating D2 receptors. These agents should be avoided when there is concern about anticholinergic side effects (such as constipation) or orthostasis, but they provide more sedation compared with high-potency agents and can be useful when symptoms predominate at night. Unlike in disorders such as depression or schizophrenia, there are no set guidelines for changing treatment in patients with delirium; however, if symptoms do not improve even somewhat after several days, it is appropriate to change class of antipsychotic.
While the proscription against benzodiazepine use is now accepted as dogma, careful use of agents such as lorazepam can be appropriate in patients with cardiac abnormalities such as prolonged QTc interval, which preclude use of neuroleptics, or if the suspected cause of delirium is serotonin syndrome, neuroleptic malignant syndrome, or alcohol withdrawal. Lorazepam can be used in conjunction with high-potency neuroleptics, such as haloperidol, for dangerous behaviors refractory to treatment. If symptoms persist beyond such combination therapy, physicians should reevaluate and re-address the underlying cause.
Given the capricious nature of delirium, conducting well-controlled and randomized trials is challenging, with ethical questions centering onconsent and logistical questions regarding how to administer a uniform intervention to patients being treated for a multitude of conditions. Breitbart et al[21] conducted the first double-blind prospective trial, which involved hospitalized AIDS patients who consented prior to the onset of delirium. The three treatment arms included a high-potency neuroleptic (haloperidol), a low-potency neuroleptic (chlorpromazine), and a benzodiazepine (lorazepam). Patients received escalating doses based on treatment response within an hour after drug administration; upon clinical response, the medication was subsequently given at the maintenance dosage. While patients who received either neuroleptic showed a response by day 2, results in the lorazepam arm were limited by significant adverse effects.
Subsequent attempts to conduct randomized controlled studies have been limited, but clinical experience has demonstrated significant limitations of pharmacotherapy. In two randomized trials, the atypical antipsychotics olanzapine[22] and quetiapine[23] have been shown to have an efficacy similar to that of haloperidol for amelioration of delirium symptoms, although neither trial specifically targeted delirium in cancer patients, and both had significant methodologic limitations.
It has been noted that older patients (> 70 years) with hypoactive delirium are less responsive to atypical antipsychotics. Finally, experience in the general psychiatric population has shown an increased risk of neuroleptic malignant syndrome in patients who receive multiple different antipsychotics. This condition, characterized by autonomic instability, fever, severe rigidity, and mental status changes, can be difficult to distinguish from other medical conditions, such as sepsis. Thus, physicians treating delirium should use monotherapy whenever possible.
A recent study by Agar et al demonstrated that patients with delirium who received haloperidol and risperidone fared worse than those who received placebo, requiring more midazolam “rescue” doses for sedation.[24] While this study demonstrated that large, well-powered, randomized controlled trials were feasible for delirium, the results raised concerns, particularly since they ran contrary to decades of clinical experience. Of note, the patients in this study were receiving only oral medications or placebo, and there were nonsignificant differences in randomization (for example, the haloperidol group was older, received higher doses of opioids prior to randomization, and were less likely to have a cancer diagnosis). However, the results do confirm that the use of antipsychotics to treat delirium still needs to be refined and adjusted. Still, by balancing judicious use of these medications with awareness of their potential side effects (Table 3), physicians can use antipsychotics in an evidence-based and safe manner.[25] As with the diagnostic workup, the treatment of delirium warrants ongoing discussion about the goals of care, with treatment tailored to comfort or cure.
Nonpharmacologic management
In addition to judicious use of antipsychotics, the National Comprehensive Cancer Network recommends nonpharmacologic measures to treat delirium.[26] These include early mobilization of the patient when appropriate; maintaining a stable day-night cycle, with limited nighttime interruption and increased daytime activity; use of orienting objects, such as clocks and calendars; limited instrumentation; and presence of staff to provide redirection, particularly overnight. Ultimately, patients and families are best served with a multidisciplinary approach. While the primary team addresses the underlying condition, psychosocial services can provide education to family members witnessing their loved one in distress; patient services can optimize the patient’s environment; and psychiatric, neurologic, and geriatric consult services can provide additional expertise. Cancer centers are typically well equipped to provide this comprehensive array of services.
While still an ominous sign, delirium is a manageable comorbidity of cancer. Given its widespread prevalence, vigilant cancer care specialists knowledgeable about delirium have the opportunity to dramatically improve the quality of care that patients receive.
Financial Disclosure: The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. de la Cruz M, Fan J, Yennu S, et al. The frequency of missed delirium in patients referred to palliative care in a comprehensive cancer center. Support Care Cancer. 2015;23:2427-33.
2. Breitbart W, Alici Y. Agitation and delirium at the end of life: “We couldn’t manage him.” JAMA. 2008;300:2898-910.
3. Meagher DJ, Moran M, Raju B, et al. Phenomenology of delirium: assessment of 100 adult cases using standardised measures. Br J Psychiatry. 2007;190:135-41.
4. Sepulveda E, Franco JG, Trzepacz PT, et al. Delirium diagnosis defined by cluster analysis of symptoms versus diagnosis by DSM and ICD criteria: diagnostic accuracy study. BMC Psychiatry. 2016;16:167.
5. Fadul N, Kaur G, Zhang T, et al. Evaluation of the Memorial Delirium Assessment Scale (MDAS) for the screening of delirium by means of simulated cases by palliative care health professionals. Support Care Cancer. 2007;15:1271-6.
6. Carpenter CR, Bassett ER, Fischer GM, et al. Four sensitive screening tools to detect cognitive dysfunction in geriatric emergency department patients: brief Alzheimer’s Screen, Short Blessed Test, Ottawa 3DY, and the caregiver-completed AD8. Acad Emerg Med. 2011;18:374-84.
7. Wada T, Wada M, Wada M, Onishi H. Characteristics, interventions, and outcomes of misdiagnosed delirium in cancer patients. Palliat Support Care. 2010;8:125-31.
8. Janelsins MC, Kesler SR, Ahles TA, Morrow GR. Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry. 2014;26:102-13.
9. Nicholas LM, Lindsey BA. Delirium presenting with symptoms of depression. Psychosomatics. 1995;36:471-9.
10. Marchington KL, Carrier L, Lawlor PG. Delirium masquerading as depression. Palliat Support Care. 2012;10:59-62.
11. Hosker C, Ward D. Hypoactive delirium. BMJ. 2017;357:j2047.
12. Farrell KR, Ganzini L. Misdiagnosing delirium as depression in medically ill elderly patients. Arch Intern Med. 1995;155:2459-64.
13. National Institute for Health and Care Excellence (NICE). Delirium: diagnosis, prevention and management (full guideline). July 2010. https://www.nice.org.uk/guidance/cg103. Accessed August 10, 2017.
14. Korc-Grodzicki B, Sun SW, Zhou Q, et al. Geriatric assessment as a predictor of delirium and other outcomes in elderly patients with cancer. Ann Surg. 2015;261:1085-90.
15. Kayser MS, Kohler CG, Dalmau J. Psychiatric manifestations of paraneoplastic disorders. Am J Psychiatry. 2010;167:1039-50.
16. Bentea G, Sculier C, Grigoriu B, et al. Autoimmune paraneoplastic syndromes associated to lung cancer: a systematic review of the literature: Part 3: neurological paraneoplastic syndromes, involving the central nervous system. Lung Cancer. 2017;106:83-92.
17. Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15:391-404.
18. Schwarzbach CJ, Schaefer A, Ebert A, et al. Stroke and cancer: the importance of cancer-associated hypercoagulation as a possible stroke etiology. Stroke. 2012;43:3029-34.
19. Isenberg-Grzeda E, Alici Y, Hatzoglou V, et al. Nonalcoholic thiamine-related encephalopathy (Wernicke-Korsakoff syndrome) among inpatients with cancer: a series of 18 cases. Psychosomatics. 2016;57:71-81.
20. Isenberg-Grzeda E, Rahane S, DeRosa AP, et al. Wernicke-Korsakoff syndrome in patients with cancer: a systematic review. Lancet Oncol. 2016;17:e142-e148.
21. Breitbart W, Marotta R, Platt MM, et al. A double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium in hospitalized AIDS patients. Am J Psychiatry. 1996;153:231-7.
22. Hu H, Deng W, Yang H, Liu Y. Olanzapine and haloperidol for senile delirium: a randomized controlled observation. Chin J Clin Rehabil. 2006;10:188-90.
23. Tahir TA, Eeles E, Karapareddy V, et al. A randomized controlled trial of quetiapine versus placebo in the treatment of delirium. J Psychosom Res. 2010;69:485-90.
24. Agar MR, Lawlor PG, Quinn S, et al. Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med. 2017;177:34-42.
25. Breitbart W, Alici Y. Evidence-based treatment of delirium in patients with cancer. J Clin Oncol. 2012;30:1206-14.
26. National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology. Distress management. Version 1.2017. http://www.nccn.org/professionals/physician_gls/pdf/distress.pdf. Accessed July 24, 2017.