Digital Gene Expression Assay Accurately Determined DLBCL Subtypes
Using a gene expression-based assay on formalin-fixed paraffin-embedded tissue, researchers were able to identify groups among DLBCL patients with significantly different outcomes from R-CHOP treatment.
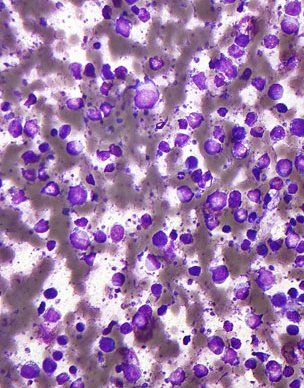
Micrograph of DLBCL, lymph node FNA specimen; copyright © 2010 Nephron
Using the gene expression-based Lymph2Cx assay on formalin-fixed paraffin-embedded tissue, researchers were able to identify groups among patients with diffuse large B-cell lymphoma (DLBCL) with significantly different outcomes after R-CHOP treatment, according to results of a recent study.
“In this first, to our knowledge, large cohort of R-CHOP–treated patients where cell of origin was determined using this assay, Lymph2Cx separated patients into groups with significantly different outcomes, independent of International Prognostic Index score and MYC/BCL2 immunohistochemistry,” researchers led by David W. Scott, MBChB, PhD, of British Columbia Cancer Research Centre, wrote in the Journal of Clinical Oncology.
Previously, cell-of-origin classification into germinal center B-cell-like (GCB) or activated B-cell-like (ABC) subtypes required fresh frozen biopsies and microarray technology. More recently, researchers have been able to use formalin-fixed paraffin-embedded tissue samples to get subtype classification. “We anticipate that over the next few years, with the emergence of agents with selective activity in ABC or GCB DLBCL, the determination of cell of origin will become part of the foundation for optimal patient care,” the authors wrote.
According to the study, recent research has shown that the digital gene expression based Lymph2Cx assay is a “highly accurate test with excellent concordance of cell-of-origin assignment.”
They conducted this analysis to demonstrate the consistency and reproducibility of cell-of-origin assignment using the Lymph2Cx assay. They applied the assay to samples from 344 patients with de novo DLBCL treated with R-CHOP. MYC and BCL2 protein expression was assessed with immunohistochemistry on tissue microarrays.
They found that the assay provided concordant cell-of-origin classifications in 96% of 49 repeatedly sampled tumor biopsies and in 100% of 83 formalin-fixed paraffin-embedded biopsies, with no observed misclassification of GCB or ABC subtypes.
Results showed that patients with ABC DLBCL had significantly worse outcomes compared with patients with GBC (P < .001) for time to progression, progression-free survival, disease-specific survival, and overall survival.
According to the study, the prognostic significance of cell of origin classification was particular evident in those patients with intermediate International Prognostic scores and the non-MYC-positive/BCL2-positive subgroups.
“Lymph2Cx is an accurate assay for DLBCL cell-of-origin assignment in widely available formalin-fixed paraffin-embedded tissue biopsies,” the researchers wrote. “In contrast to results obtained with immunohistochemistry, the consistency of this assay provides the opportunity to bring uniformity to how these gene expression profiling (GEP)-defined subtypes are assigned and subsequently studied.”
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.