Drug Combo Could Overcome Resistance in Mantle Cell Lymphoma
A combination of the CDK4 inhibitor palbociclib with ibrutinib in mantle cell lymphoma could potentially overcome the drug resistance that many patients face.
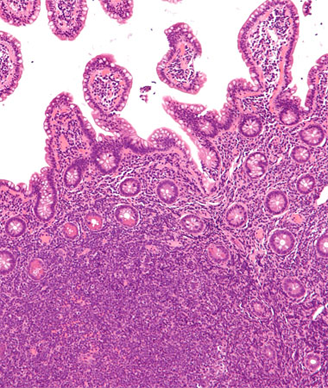
Intermediate magnification micrograph of mantle-cell lymphoma of the terminal ileum; Copyright © 2010 Nephron
Ibrutinib (Imbruvica) is an oral therapy that targets and inhibits the Bruton tyrosine kinase (BTK), which is found active in several types of B-cell malignancies, including mantle cell lymphoma (MCL). Ibrutinib is approved by the US Food and Drug Administration for MCL patients, yet about one-third of these patients do not respond to the treatment and those that do often become resistant to the drug. There are yet no targeted therapies to treat these relatively frequent cases.
Now, using genomic sequencing and RNA expression analyses of both tumor and healthy patient tissue, researchers may have found the molecular mechanism by which MCL either does not respond to a BTK inhibitor, or initially responds but then develops resistance.
The researchers identified a specific mutation, C481S, in patients who initially had a durable response to ibrutinib but then progressed. According to the researchers, this is the first patient-relapse–specific mutation to ibrutinib in MCL identified. The C481S mutation resulted in increased BTK activation as well as AKT activation that were driven by the cell-cycle regulator CDK4. The mutation appears to be specific to those patients who had prolonged exposure to ibrutinib as no de novo resistance patients harbored this mutation nor did those patients who only transiently responded to ibrutinib therapy.
The results are published in Cancer Discovery.
David Chiron, PhD, Selina Chen-Kiang, PhD, both of the department of pathology and laboratory medicine at the Weill Cornell Medical College in New York City, and colleagues analyzed serial biopsies and healthy tissue samples from five MCL patients using whole-exome and whole transcriptome sequencing. All of the patients had initially responded to ibrutinib therapy before developing resistance. The C481S mutation was detected in two of these patients, one of whom had a durable partial response to ibrutinib for 30 months. The study also analyzed six patients who had either primary resistance to ibrutinib or a partial response of less than 5 months.
MCL cells from a single patient with the BTK C481S mutation had higher BTK activation, greater genomic instability, CDK4-driven proliferation in the spleen, and increased PI3K-AKT pathway signaling. Prior studies have shown that the PI3K pathway is necessary for the development of the B-cell lineage and for its proliferation. This pathway acts upstream of BTK in mature B cells.
“The knowledge that we gained from longitudinal RNA and genomic sequencing of mantle cell lymphomas with primary and acquired resistance to ibrutinib allowed us to identify rational drug combinations that may overcome resistance in these two settings,” said Chen-Kiang in a statement.
Blocking CDK4 with the targeted CDK4 inhibitor palbociclib in BTK C481S lymphoma cell lines resulted in these cells being sensitive to PI3K inhibitors.
“Targeting CDK4 with palbociclib in combination with PI3K or BTK inhibition is poised for clinical validation in MCL,” said the authors in their discussion. “Palbociclib had already achieved a durable clinical response with a favorable toxicity profile in the first single-agent clinical trial in patients with recurrent MCL.”
The researchers have recently opened a clinical trial to test palbociclib and ibrutinib in this patient population (NCT02159755).
This study was funded by the Lymphoma Research Foundation, the Lymphoma Foundation, the Cancer Research and Treatment Fund, the Leukemia and Lymphoma Society, as well as the National Cancer Institute.
Targeted Therapy First Strategy Reduces Need for Chemotherapy in Newly Diagnosed LBCL
December 7th 2025Lenalidomide, tafasitamab, rituximab, and acalabrutinib alone may allow 57% of patients with newly diagnosed LBCL to receive less than the standard number of chemotherapy cycles without compromising curative potential.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.