Durable Responses Seen With Pembrolizumab in Melanoma Patients
Data from the KEYNOTE-001 study showed that the anti–PD-1 antibody pembrolizumab produces durable responses in metastatic melanoma patients.
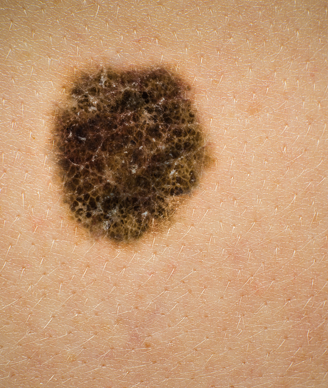
Image © Australis Photography / Shutterstock.com
Long-term data from the KEYNOTE-001 study showed that the anti–programmed death 1 (PD-1) antibody pembrolizumab produces durable responses in metastatic melanoma patients. These results were presented (abstract 9005) at the 2015 American Society of Clinical Oncology (ASCO) Annual Meeting held May 29 to June 2 in Chicago, by Adil Daud, MD, director of melanoma clinical research at the University of California, San Francisco Helen Diller Family Comprehensive Cancer Center.
Pembrolizumab is approved as a second-line therapy for metastatic melanoma following treatment with either ipilimumab or, for patients with BRAF-mutated tumors, an oral BRAF inhibitor at a dose of 2 mg/kg every 3 weeks. Thus far, more than 2,000 melanoma patients have been evaluated in clinical trials with pembrolizumab.
The overall response rate was 34% and the complete response rate was 6%. Eighty percent of responses were still ongoing at the time of analysis, and the median duration of response has not yet been reached.
The median progression-free survival (PFS) was 4.4 months; the PFS rate at 12 months was 34%. The median overall survival was 22.8 months. The 1- and 2-year overall survival rates were 66% and 49%, respectively.
Among 152 treatment-naïve metastatic patients, the median PFS was 13.8 months and the median overall survival was 31.1 months. The complete response rate in this patient subpopulation was 17.8% and the overall response rate was 50%.
“The safety of pembrolizumab over a longer-term period was good, the responses were durable, and in both treatment-naïve BRAF-mutant–positive and –negative patients, the overall response rate was high,” Daud told Cancer Network. “The low incidence of grade 3 and 4 toxicity is notable in this large patient population,” he added.
Patients received one of three doses of pembrolizumab (2 mg/kg every 3 weeks, 10 mg/kg every 3 weeks, or 10 mg/kg every 2 weeks). Patients were assessed every 3 months after discontinuation of therapy.
Of the 655 patients on the study, 342 were previously treated with ipilimumab and 313 were ipilimumab-naïve. The median patient follow-up period was 14.8 months and the median duration of drug exposure was 5.6 months.
The patients had a median age of 61 years. Seventy-eight percent had advanced disease with visceral metastases.
At the time of analysis, 33% (217) of patients were still on therapy. Response rates were 29% and 38% in the ipilimumab-treated and -naïve patients, respectively.
High-grade adverse events were seen in 14% of patients; there were no therapy-related deaths on the study. The most frequent any-grade adverse events were hypothyroidism (7.5%), hyperthyroidism (2.3%), pneumonitis (2.7%), and colitis (1.7%). Grade 3 or 4 colitis occurred in 1.1% of patients.
Of the 411 patients who could be evaluated for PD-ligand 1 (L1) expression on their tumors, PD-L1–positive patients were more likely to respond to pembrolizumab (P < .0001).
Based on these and other data, pembrolizumab should be an option for treatment-naïve metastatic melanoma patients, Daud concluded.