Elders With Lenalidomide-Refractory Myeloma May Lack Optimal Treatments
A real-world study assessed treatment patterns and outcomes of elderly patients with lenalidomide-refractory multiple myeloma after 1 to 3 therapy lines.
A real-world study assessed treatment patterns and outcomes of elderly patients with lenalidomide-refractory multiple myeloma after 1 to 3 therapy lines.
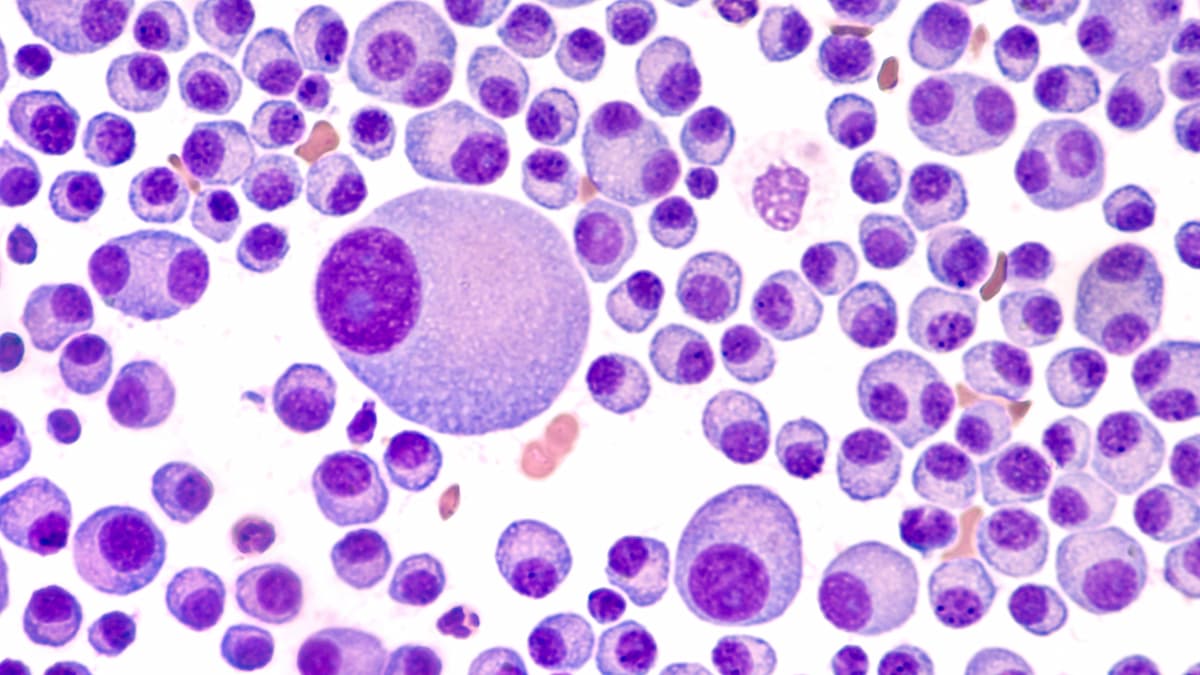
Population-based data on patients 65 years or older, 81% of whom had at least 1 NCI comorbidity, with lenalidomide (Revlimid)-refractory multiple myeloma treated with 1 to 3 prior lines of therapy revealed poor survival outcomes and rapid therapy progression, suggesting the need for new therapeutic options, according to findings from a real-world study published in Clinical Lymphoma, Myeloma, and Leukemia.
Data from the trial revealed that the median overall survival (OS) for all patients included in the analysis was 29.3 months (95% CI, 25.1-33.9), with OS decreasing with increasing lines of prior therapy. In patients who underwent 1, 2, and 3 prior lines of therapy, the median OS was 53.0 months (95% CI, 36.4-not estimable [NE]), 20.7 months (95% CI, 17.3-27.1), and 19.0 months (95% CI, 17.2-23.7), respectively.
Additional data reveal a similar trend in the time to next treatment (TTNT) or death, with more lines of prior therapy associated with decreased TTNT or death. Overall median TTNT or death was 8.5 months (95% CI, 7.7-9.7) vs 11.0 months (95% CI, 9.5-12.7) in patients who had 1 previous line of therapy. Additionally, the median TTNT or death in those who had 2 and 3 prior lines of therapy was 7.2 months (95% CI, 6.6-8.3) and 6.1 months (95% CI, 5.5-7.9), respectively.
“[T]hese population-based data on elderly patients [81% with at least 1 of the NCI comorbidities] and early-line lenalidomide-refractory disease add to the nascent body of real-world evidence describing their outcomes since the introduction of daratumumab [Darzalex],” Binod Dhakal, MD, MS, associate professor of Medicine, Division of Hematology at Froedtert Hospital and the Medical College of Wisconsin, wrote in the publication with study coinvestigators. “Poor survival and rapid progression through therapies in this difficult-to-treat patient population highlight the shortcomings of currently available therapies and the need for new and effective therapeutic options.”
The study assessed 1297 patients from the SEER cancer registry with multiple myeloma who had proteasome inhibitor and immunomodulatory drug exposure, lenalidomide-refractory disease, and 1 to 3 prior lines of therapy indexed between 2016 and 2020. The median age was 75 years (IQR, 71-79), 88% of patients were White, and 54% of patients were male. Additionally, the median time from diagnosis to index date was 22.0 months (IQR, 11.7-34.5).
A total of 22% of patients received stem cell transplantation. Most patients received 1 prior line of therapy (52%), with 34% having received 2 prior lines, and 13% having received 3 prior lines. In addition to lenalidomide, patients were also previously treated with bortezomib (Velcade, 94%), carfilzomib (Kyprolis, 13%), daratumumab (9%), ixazomib (Ninlaro, 8%), and thalidomide (Thalomid, 1%). Furthermore, the mean NCI comorbidity index score was 0.87 (SD, 0.74), with the most prevalent comorbidities including renal disease (42%), diabetes (31%), chronic pulmonary disease (28%), and congestive heart failure (28%).
Singlet, doublet, and triplet regimens were used in 32%, 34%, and 31% of patients on study. The most common drugs used during index treatment included daratumumab (43.7%) and pomalidomide (Pomalyst; 43.3%), followed by bortezomib (25.5%), carfilzomib (19.0%), and ixazomib (12.2%). Of note, daratumumab and pomalidomide use increased with exposure to more lines of therapy. From 2016 to 2020, daratumumab use increased from 8.1% to 53.0%, and pomalidomide use increased from 40.4% to 41.8%. Alternatively, bortezomib use decreased during the same period, from 28.7% in 2016 to 24.8% in 2020.
The study assessed OS and TTNT or death, with TTNT defined as the time from first index date to the initiation of the next line of treatment or death.
Reference
Dhakal B, He J, Schecter JM, et al. Real-world treatment patterns and outcomes in patients with lenalidomide-refractory multiple myeloma with 1 to 3 prior lines: SEER-Medicare database. Clin Lymphoma Myeloma Leuk. Published January 23, 2025. doi:10.1016/j.clml.2025.01.009
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.