Endometrial Cancer at Young Age Ups Risk for Colorectal Cancer
Women diagnosed with endometrial cancer at age 50 or younger had a fourfold increased risk for a subsequent colorectal cancer diagnosis, according to a historical cohort study published recently in the Journal of Clinical Oncology.
Women diagnosed with endometrial cancer at age 50 or younger had a fourfold increased risk for a subsequent colorectal cancer diagnosis, according to a historical cohort study published recently in the Journal of Clinical Oncology.
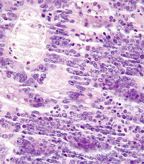
Very high magnification micrograph of tumor infiltrating lymphocytes in a case of colorectal carcinoma; Copyright © 2012
Nephron
“Identification of individuals at a higher risk of colon cancer than the general population is an important aspect of colon cancer screening and can help develop tailored approaches to colon cancer screening,” Harminder Singh, MD, of the University of Manitoba and CancerCare Manitoba, Winnipeg, Canada. “Screening for colon cancer with colonoscopy should be considered after diagnosis of endometrial cancer in all age groups and molecular evaluation for Lynch syndrome, especially when endometrial cancer is diagnosed before age 50.”
Singh and colleagues linked data from the Manitoba Cancer Registry and the Manitoba administrative health databases in an attempt to discover the site-specific risk for colorectal cancer among women who had prior diagnosis of endometrial cancer.
Their study included 3,115 women with endometrial cancer and 15,084 age-matched women without invasive cancer. Each patient was followed until diagnosis of colorectal cancer or another cancer, death, migration, or study end. The patients were followed for 145,502 person-years. Median age at diagnosis with endometrial cancer was 64 years.
No overall difference in the likelihood of colorectal cancer diagnosis was found between the two groups (1.9% in endometrial survivors vs 1.6% for healthy controls).
However, when the researchers stratified patients by age, a difference in risk for colorectal cancer emerged. Specifically, those women diagnosed with endometrial cancer at age 50 or younger had a hazard ratio (HR) of 4.41 for a diagnosis of colorectal cancer (95% CI, 1.47–13.26). In contrast, women diagnosed with endometrial cancer at age 51 to 65 or older had no significantly increased risk for all colorectal cancers.
The researchers also looked at colorectal cancer risk by site and found that women diagnosed with endometrial cancer at age 50 or younger had a HR of 7.48 (95% CI, 1.29–43.30) for diagnosis with right-sided colorectal cancer. In addition, women age 51 to 65 also had an increased risk for diagnosis with right-sided colorectal cancer (HR = 2.30; 95% CI, 1.05–5.01).
“A higher proportion of colon cancers occur in the right colon in women, as compared to that in men, and exposure to estrogens may be responsible for this finding,” Singh told Cancer Network. “Estrogens have also been implicated in the etiopathogenesis of endometrial cancer and may be increasing the risk of right-sided colon cancer among women with history of endometrial cancer.”