Enzyme Plays Dual Tumor Suppressive Role in Kidney Cancer
Researchers have identified a key gluconeogenic enzyme, the absence of which in clear cell renal cell carcinoma (RCC) may explain the uncontrolled cell growth present in cancer cells compared with normal kidney cells.
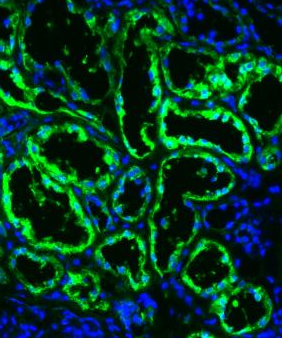
A metabolic enzyme has an unexpected role in regulating gene expression in kidney cancer. Image of primary human kidney tissue: FBP1 protein (green); cell nuclei (blue). Credit: Bo Li and Brian Keith, Perelman School of Medicine, University of Pennsylvania.
Researchers have identified a key gluconeogenic enzyme, the absence of which in clear cell renal cell carcinoma (RCC) may explain the uncontrolled cell growth present in cancer cells compared with normal kidney cells.
This discovery was made by Celeste Simon, PhD, professor of cell and developmental biology and scientific director of the Abramson Family Cancer Research Institute at the University of Pennsylvania, and colleagues, who published the results of their study in Nature.
Clear cell RCC is characterized by elevated glycogen and fat deposits in affected kidney cells. This over-storage of lipids is caused by a faulty series of biochemical reactions, called the Krebs cycle. Patients with clear cell RCC have a hyperactive Krebs cycle, resulting in enhanced lipid production. In addition, renal cancer cells are associated with both elevated expression of hypoxia inducible factors (HIFs) and mutations in the bon Hippel-Lindau (VHL) encoded protein, pVHL.
According to background information in the study, studies have shown that deletion of VHL alone did not produce clear cell RCC specific tumor formation in mice, suggesting that there may be additional mechanisms at play. Recent studies have shown that changes within the cell nucleus may account for kidney tumor progression.
Therefore, in their study, Simon and colleagues used pan-metabolic profiling and metabolic gene set analysis to analyze the metabolic enzymes in more than 600 tumor samples, and found that fructose-1,6-bisphosphatase 1 (FBP1), an enzyme essential for regulating metabolism, was depleted in almost 100% of the clear cell renal cell carcinoma samples.
“Notably, the human FBP1 locus resides on chromosome 9q22, the loss of which is associated with poor prognosis for clear cell RCC patients,” the researchers wrote.
Further study, showed that when FBP1 binds with HIF in normal cells, it suppressed clear cell RCC and other tumor cell growth. However, in cells with FBP1 depletion, the researchers observed the Warburg effect, a phenomenon in which malignant, rapidly growing tumors cells produced energy up to 200 times faster than normal cells.
Simon and colleagues also found that in cells deficient of pVHL, FBP1 restrained “cell proliferation, glycolysis and the pentose phosphate pathway in a catalytic-activity-independent manner, by inhibiting nuclear HIF function via direct interaction with the HIF inhibitory domain.”
This unique dual function of FBP1 explains its ubiquitous loss in clear cell RCC, distinguishing FBP1 from previously identified tumor suppressors that are not consistently inhibited in all tumors.
“Collectively, our data reveal an intriguing regulatory relationship between FBP1 and hypoxic responses in renal carcinoma, which has implications for the metabolic regulation of all gluconeogenic tissues,” the researchers wrote.