EUTOS Score Validated for Predicting Treatment Outcomes With TKI Therapy
A new study validates a simple prognostic score, the EUTOS score, as a useful tool in predicting the therapeutic effects of TKIs for chronic myeloid leukemia.
While tyrosine kinase inhibitors (TKIs) have revolutionized the treatment of chronic myeloid leukemia (CML) in recent years, prognosis of the disease and prediction of response to those treatments has fallen behind. A new study validates a simple prognostic score known as the EUTOS score, featuring only two variables, as a useful tool in prediction of therapeutic effects of TKIs, and especially of imatinib.
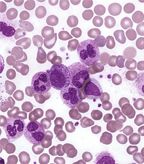
CML; source: Robert Cardiff, PhD
Before TKIs were developed, the Sokal risk score was developed and used for patients receiving conventional chemotherapy for CML. In the era of interferon-alfa treatment, the Euro risk score was established. But the rapid development and adoption of imatinib and other TKIs did not bring another score system with it, and the Sokal and Euro scores were still used.
The EUTOS score, developed in 2011, is based on analysis of the European Treatment and Outcome Study for CML; in that study, a score including only spleen size and blood basophil percentage predicted complete cytogenetic response (CCyR) within 18 months of imatinib initiation and progression-free survival better than the earlier scores could.
The EUTOS score is arrived at by adding seven times the basophil percentage in peripheral blood and four times the spleen size, measured in centimeters (maximum distance below the costal margin, by manual palpation). If the EUTOS score is 87 or below, the patient is considered low-risk; above 87 places the patient in the high-risk category.
In a new validation study, researchers led by Verena S. Hoffmann, MA, of Ludwig-Maximilians-Universitt in Munich, confirmed the EUTOS score’s utility in 1,288 patients treated with first-line imatinib outside of prospective randomized trials. Among 1,251 evaluable patients, 161 (12.5%) had a EUTOS score higher than 87, placing them in the high-risk category. Those high-risk patients had a significantly lower cumulative incidence of ever achieving a CCyR, at 67.6% vs 84.4% in low-risk patients at 5 years (P < .0001). The probability of being in CCyR after 18 months was 61.3% for high-risk patients and 73% for low-risk patients.
Progression-free survival was also significantly lower in the high-risk group (P = .0395). After 5 years, progression-free survival was 89.3% in the low-risk patients and 82% in the high-risk group.
The authors wrote that while a number of genetic prognostic markers are under consideration, the data are not yet mature enough to be used universally. “The EUTOS score has now been validated in many independent studies” in spite of an unclear mechanism that underlies the relationship between basophils, spleen size, and treatment outcome. “In the era of molecular hematology, this may be seen as puzzling or even frustrating, but until new, biological factors are identified and validated-including particularly the gene expression profile-it will be difficult to improve further on the prognostic assessment of CML before a treatment is initiated.”